INDT-EPI Module for Epilepsy
Objectives of The Module
- Overview of Childhood epilepsy and its classification
- Describe various clinical presentations of Childhood Epilepsy
- Description of INDT-EPI tool
- Clinically evaluate the child with epilepsy using INDT-EPI tool
- Future research : Need for modified tool
Practical Definition of Epilepsy
- Epilepsy is a disease of the brain defined by any of the following condition
- At least two unprovoked (or reflex) seizures occurring >24 h apart
- 2.One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years
- Diagnosis of an epilepsy syndrome
Epilepsia, 55(4):475–482, 2014
What is not Epilepsy ?
- Non-epileptic event
- Breath holding spells
- Syncope
- Pseudo seizures
- Provoked seizures
- Febrile seizures
- Following head trauma (within 7 days)
- During acute phase of CNS infections
- Metabolic disturbances –hypoglycemia, hypocalcemia, hyponatremia, hypoxia
Classification of Epilepsy

Epilepsia, 52(6):1058–1062, 2011
Classification of Epilepsy

Epilepsia, 52(6):1058–1062, 2011
Febrile Seizures
- Commonly seen in infancy and early childhood between the ages of 3 months to 6 years
- Can be aassociated with a systemic febrile illness but without any evidence of infection of the CNS
- Simple febrile Seizure
- Generalized, brief (< 15 min), within 24 hours of onset of fever, single episode
- Complex Febrile seizure
- focal onset, duration more than 15 minutes, associated focal neurological deficits or multiple episodes in the same illness
- Simple Febrile Seizure Plus
- recurrent episodes of febrile seizures within 24 hours which otherwise behaves like simple febrile seizures.
Status Epilepticus
- Seizure lasting for >30 min or recurrent seizures for >30 min during which the child does not regain consciousness in between the seizures
- Operational Definition
- A child who is brought to the physician from an extramural setting still convulsing should be considered to be in status epilepticus
- the minimum time for this definition of status epilepticus is regarded as more than 5 minutes
- A prolonged seizure → brain damage
- Imperative to control seizures as soon as possible
Focal Seizures
Legend: Observe the baby having seizures starting from left side in the form of eyelid flickering and dystonic posturing of left upper limb progressing to involve all four limbs
Absence Seizures
Legend: Observe the girl getting blank (sudden behavioral arrest) for few seconds following hyperventilation suggestive of absence seizure
Infantile Spasms
Legend: Observe the baby having sudden flexion of head with embracing movement of both upper limb suggestive of flexor spasms or 'salaam' spel
Infantile Spasms
Legend: Observe the baby having extensor epileptic spasms in cluster
Head Drop
Legend: Observe the child having episodes of sudden head drops
Other Movement
Legend: Observe the tremulous movement of body (infantile tremor syndrome)
Legend: observe the coarse tremors of the outstretched hands
Neurocutaneous Markers

CO-MORBIDITIES
- Intellectual disability
- Behavioural disturbances
- Cerebral palsy
- Autism
- Vision impairment
- Hearing impairment
- Attention-Deficit/Hyperactivity Disorder
- Feeding difficulties
Misdiagnosis of Epilepsy
Seneviratne U et al Epilespia2012;53:e63-6.
Paroxysmal Nonepileptic events (PNEE)
- Misdiagnosis may lead to inappropriate and potentially harmful treatments
- Distinguishing between epileptic and non epileptic events simulating seizures is essential
- Frequently encountered in day to day practice and large number of discrete entities
- Taking a thorough history is the most crucial part of any evaluation in addition to a careful observation
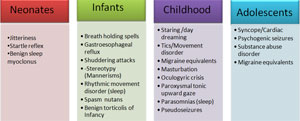
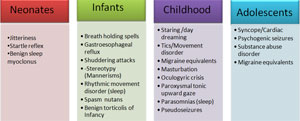
PNEE-Age Based Causes
Breath Holding Spells
- 6 months – 2 years (up to 5 years)
- Typically confused with tonic seizure
- Always a trigger: fear, injury, frustration
- Sequence: Cry → breath holding (expiration) → cyanosis/paleness → stiff, loss of awareness → clonic jerks
- Correction of anemia, counseling
- Pallid type (Reflex asystole)
- parasympathetic dysregulation, pale and limp, with asystole
Gastroesophageal Reflex
- Dystonic, abnormal movements of head,neck, upper trunk (Sandifer's syndrome)
- Life-threatening events – apnea with cyanosis and/or pallor
- Vomiting, failure to thrive
- More common in delayed/hypotonic patients
- Management: Confirm diagnosis, treatment of reflux

Ophisthotonus Posturing Final Diagnosis- Nemaline Rod Myopathy
Shuddering Attacks (Stereotypy)
- Onset 6 m–10 yrs, gradually better
- Sudden tremulous contraction (shiver)
- Flexion of head and trunk
- Adduction and flexion of elbows
- Brief, up to 100/day, cluster
- Intervening several weeks of no spells
- Benign phenomenon
- No treatment, gradually disappears
- Specific stereotypy/mannerism
Tics
- Repetitive, Purposeless movements
- Sudden, brief, stereotypic, wax/wane
- Brief voluntary inhibition possible
- Worsen with anxiety, Disappear in sleep
- Motor Tics
- Simple: Face twitch, head shake, eye blink, sniff
- Complex: Facial distortion, jump, fiddle, sway
- Vocal: cough, clear throat, words (profane)
- Common: Tourette syndrome
Syncope
- Transient global cerebral hypoperfusion
- Pre-syncopal symptoms (aura)
- light head, nausea, visual blurring, distant hearing, vertiginous
- Syncope:
- Fall/slump, pale, loss of awareness, stiff, clonic jerking (confused with GTCS)
- Three most common in children
- Vasovagal (Neuro-cardiogenic)
- Orthostatic (Drugs, autonomic dysfunction)
- Cardiogenic (Arrhythmia)
Psychogenic Non Epileptic events(PNEE)
- Episodic behavioral events that mimic epileptic seizures but are not associated with abnormal cortical electrical discharges.
- Related to an underlying psychological stressor or conflict and differ from other paroxysmal nonepileptic events
- Use of the term “seizures” for these events adds to confusion
- Psychogenic non epileptic events” (indicates non epileptic nature of these attacks )
House Tree Person Test for PNEE
- HTP is a projective personality test
- Test taker responds to ambiguous, abstract, or unstructured stimuli (often in the form of pictures or drawings)
- Measures aspects of a person's personality through interpretation of drawings and responses to questions
- Fortifies unconscious/conscious conflicts and stressors
HTP

Burden of Epilepsy in INDIA
- INCLEN study group has shown overall epilepsy prevalence estimate of 1.75 (95% CI-1.39-2.20)
- Rural India has epilepsy prevalence estimate of 1.70 (95% CI-1.29-2.24)
- Urban population has prevalence estimate of 1.93 (95% CI-1.27-2.94).
Treatment Gap
- Defined by ILAE as the difference*
- between the number of people with active epilepsy (defined in this case as two or more unprovoked seizures on different days in the previous year)
- the number whose seizures are being appropriately treated in a given population at a give point in time, expressed as a percentage
- In India treatment gap is varying from 30-70% more in rural areas compared to semiurban and urban areas.#
*Meinardi H et al. Epilepsia 2001; 42: 136–49.
#Pandey S at Al. Journal Of Tropical Pediatrics, 2013
Gourie-Devi M et al, Epilepsia 2003; 44: 58–62.
Ray BK et al,J Indian Med Assoc 2002; 100: 322–26
Is Diagnostic tool Necessary?
- Validated and culturally adapted Indian tool to diagnose epilepsy required in resource limited settings
- Early diagnosis and prompt treatment/referral can be made by primary health care provider
- Training of primary health care provider: Reduce the burden on tertiary health care systems and allow appropriate, judicious and cost-effective use of available resources
Consensus clinical criteria
A child will be diagnosed as having epilepsy
Only if
He/ she has history of 2 or more unprovoked
seizures beyond 28 days of life
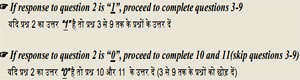
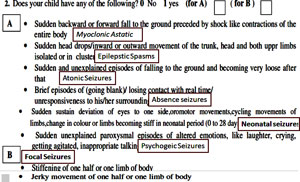
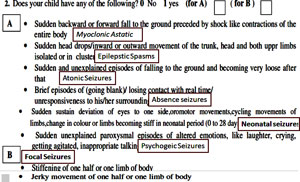
Overview of INDT-EPI tool
- INDT-EPI included questions in simple language: 13 questions
- Elicit the history of common seizure types
- Generalized and partial motor seizures
- Absence seizures
- Myoclonic seizures (questions 1,2,10,11)
- Number of seizures (question 3)
- Duration between first and last seizures (Question 4)
Overview of INDT-EPI tool
- Provoked seizures such as febrile seizures (Question 5)
- Seizures occurring during neuro-infections (Question 6), head trauma or during systemic illnesses
- Neonatal seizures (Question 7)
- Seizure mimics such as breath holding spells (question 8) and syncopal attacks (question 9).
- Question 12 and 13 are final diagnosis.
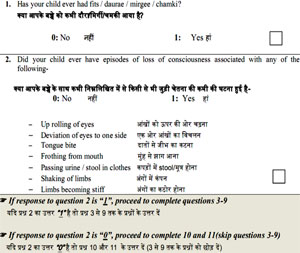
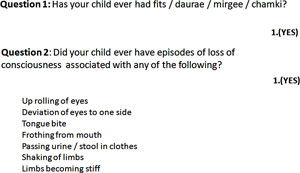
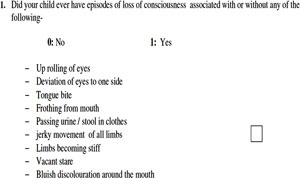
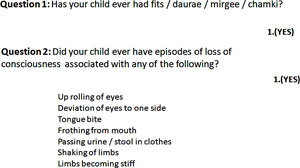
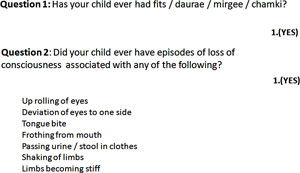
INDT-EPI tool: Question 1
- Question 1: Has your child ever had fits / daurae / mirgee / chamki?
- Mark YES: If Parents say that the child has had fits / daurae / mirgee / chamki
- Mark NO: If child never had seizure
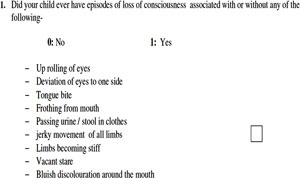
Question 2
Did your child ever have episodes of loss of consciousness associated with any of the following?
- Up rolling of eyes
- Deviation of eyes to one side
- Tongue bite
- Frothing from mouth
- Passing urine / stool in clothes
- Shaking of limbs
- Limbs becoming stiff
- Mark YES: If the child had loss of consciousness with at least one of the associated features
- Mark NO: If the child never had loss of consciousness OR child had loss of consciousness, but not associated with any of the seven listed features
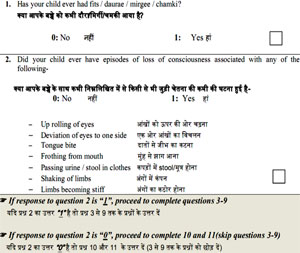
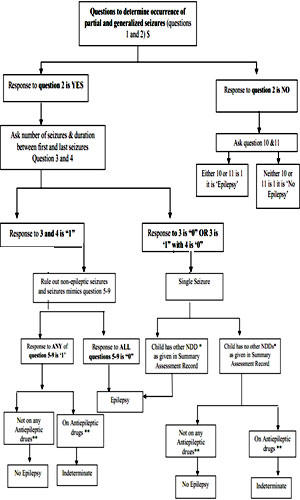
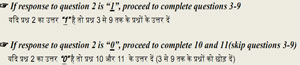
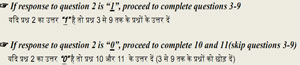
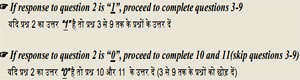
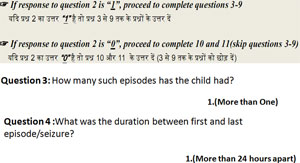
If the answer to Question 2 is 'Yes', then complete questions 3-9; otherwise go to question 10
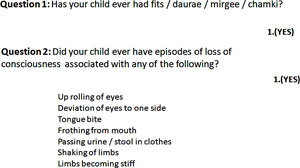
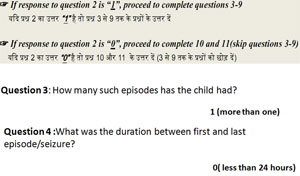
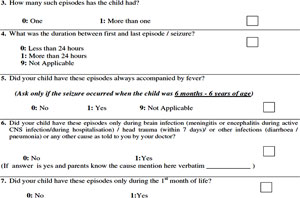
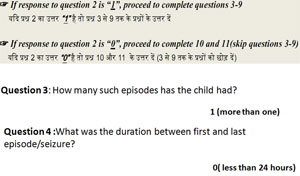
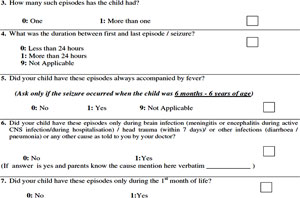
Question 3
- How many such episodes has the child had?
- Mark “0”: If the child has had only ONE episode/seizure.
- Mark “1”: If the child has had MORE THAN ONE episode/seizure.
Question 4
- What was the duration between first and last episode/seizure?
- Mark “0”: If the child has had two or more seizures but LESS THAN 24 hrs apart.
- Mark “1”: If the child has had two or more seizures MORE THAN 24 hrs apart.
- Remember, according to the CCC for epilepsy, “2 or more unprovoked seizures at least 24 hours apart” will be classified as Epilepsy. Questions 3 and 4 elicit this information.
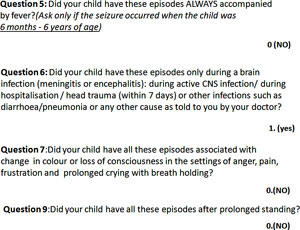
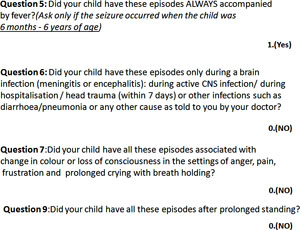
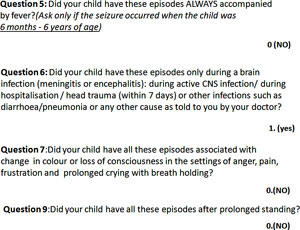
Question 5
- Did your child have these episodes ALWAYS accompanied by fever? (Ask only if the seizure occurred when the child was 6 months - 6 years of age)
- How to ask: Emphasise “ALWAYS”
- Mark YES: If child has/had seizures ALWAYS accompanied by fever
- Mark NO: If child's seizures were NOT accompanied by fever
- Child has/had seizures accompanied by fever AND ALSO seizures not accompanied by fever (Febrile and a febrile seizures occurring together)
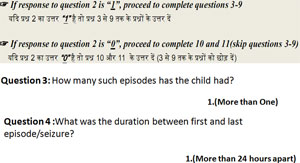
Question 6
- Did your child have these episodes only during a brain infection (meningitis or encephalitis): during active CNS infection/ during hospitalisation / head trauma (within 7 days) or other infections such as diarrhoea/pneumonia or any other cause as told to you by your doctor?
- Mark YES: If child had seizures due to some identifiable cause and within the 7 days of that insult/event as listed in the description
- Mark NO: If seizures were not related to any identifiable cause
Question 7
- Did your child have these episodes ONLY during 1st month of life?
- Mark YES: If child had seizures ONLY during the neonatal period
- Mark NO: If child did not have seizures during the neonatal period OR
- If the child had seizures during AND beyond the neonatal period also OR
- If the child had seizures only after the neonatal period
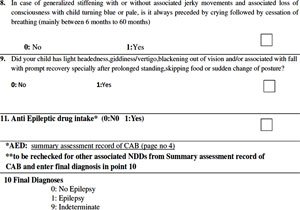
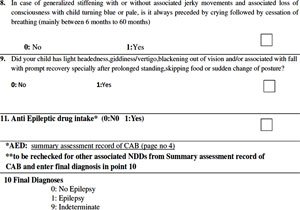
Question 8
- Did your child have all these episodes associated with change in colour or loss of consciousness in the settings of anger, pain, frustration and prolonged crying with breath holding? (May add colloquial terms for Breath holding spells)
- How to ask: Emphasise “PROLONGED CRYING”, “BREATH HOLDING” and turning blue.
- Mark YES: If the child had episodes of breath holding as described above
- Mark NO: If the child never had breath holding spells
Question 9
- Did your child have all these episodes after prolonged standing?
- How to ask: Emphasis should be on “prolonged standing”
- Mark YES: If child had episodes of fainting or unconsciousness after prolonged standing
- Mark NO: If child has never had such episodes
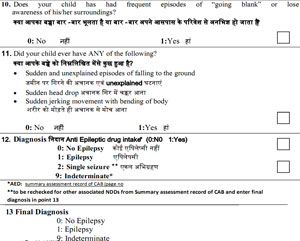
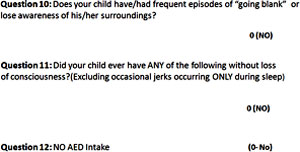
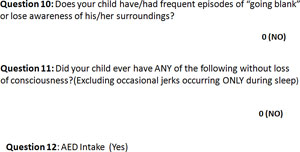
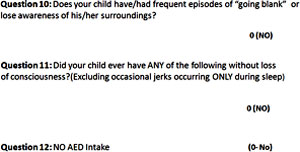
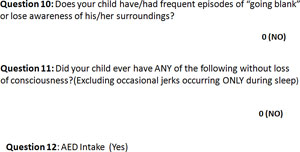
Question 10
- Does your child have/had frequent episodes of “going blank” or lose awareness of his/her surroundings?
- YES: Child had frequent episodes of “going blank” OR Child had frequent episodes of “losing awareness of surroundings”
- NO: Child never had episodes of “going blank”/ “losing awareness of surroundings”
- Presence of absence seizures can be often confirmed by asking the child to hyperventilate. However, failing to elicit absence seizures by hyperventilation does not rule out it.
Question 11
- Did your child ever have ANY of the following without loss of consciousness? (Excluding occasional jerks occurring ONLY during sleep)
- Sudden and unexplained episodes of falling to the ground
- Sudden head drop
- Sudden jerking movement with bending of body
- Mark YES: If child had or continues to have any form of myoclonic jerks as described above without loss of consciousness
- Mark NO: If child never had abnormal jerky movements / head drop / sudden unexplained fall to ground OR
- Occasional jerks occurring only during sleep
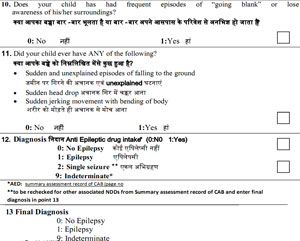
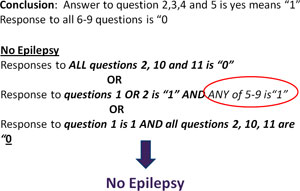
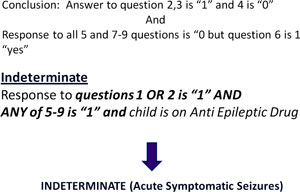
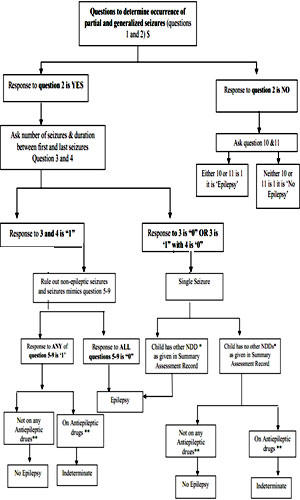
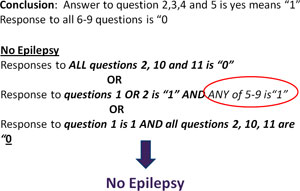
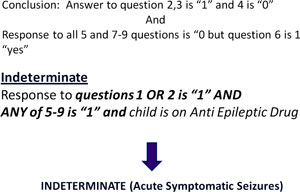
Interpretation and Diagnosis
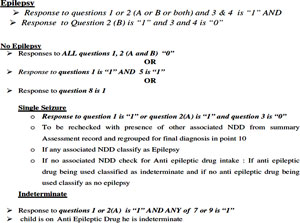
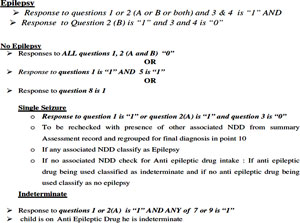
Epilepsy
- Response to ALL questions 2, 3 and 4 is "1" AND response to ALL of the questions 5-9 is "0"
AND / OR
- Response to either/both of the questions 10 or 11 is 1
Interpretation and Diagnosis
Single Seizure
Response to question 2 is "1" AND question 3 is "0" AND
response to all of the question 5-9 is "0"
- If any associated NDD classify as Epilepsy
- If no associated NDD check for Anti epileptic drug intake: If anti epileptic drug being used classified as indeterminate and if no anti epileptic drug being used classify as no epilepsy
Interpretation and Diagnosis
- Indeterminate
- Response to questions 1 OR 2 is “1” AND ANY of 5-9 is “1” and child is on Anti Epileptic Drug he is indeterminate
- In case of single seizures as detailed above
Algorithm for Assessment of Epilepsy
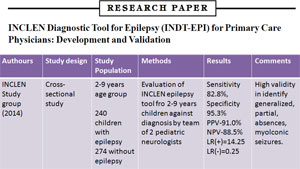
Validation of INCLEN tool
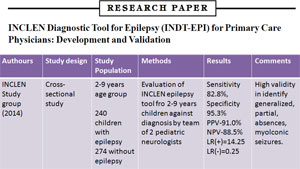
Indian Pediatrics, Volume 51,July 15, 2014
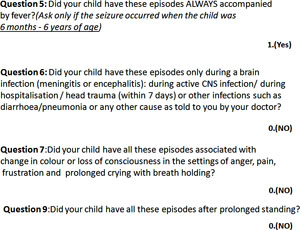
Case Vignette
- 7 year old girl visited OPD with history of unprovoked 2 episodes of unconsciousness in last 3 months.
- Both episodes occurred during sleep with sudden onset of deviation of eyes one side, facial twitching and gurgling sounds associated with stiffening of all four limbs with loss of consciousness.
- Each episode was lasted for 3-5 minutes followed by postictal confusion up to 30 minutes
- Birth history and developmental history was normal. No family history of seizures
Question 1: Has your child ever had fits / daurae / mirgee / chamki?
1.(Yes)
Question 2: Did your child ever have episodes of loss of consciousness associated with any of the following?
- Up rolling of eyes
- Deviation of eyes to one side
- Tongue bite
- Frothing from mouth
- Passing urine / stool in clothes
- Shaking of limbs
- Limbs becoming stiff
1.(Yes)
Question 3: How many such episodes has the child had?
1.(More than One)
Question 4: What was the duration between first and last episode/seizure?
1.(More than 24 hours apart)
Question 5: Did your child have these episodes ALWAYS accompanied by fever? (Ask only if the seizure occurred when the child was
6 months - 6 years of age)
0.(NO)
Question 6: Did your child have these episodes only during a brain infection (meningitis or encephalitis): during active CNS infection/ during
hospitalisation / head trauma (within 7 days) or other infections such as
diarrhoea/pneumonia or any other cause as told to you by your doctor?
0.(NO)
Question 7: Did your child have all these episodes associated with change in colour or loss of consciousness in the settings of anger, pain,
frustration and prolonged crying with breath holding?
0.(NO)
Question 9: Did your child have all these episodes after prolonged standing?
0.(NO)
Final Diagnosis
Answer to question 2,3 and 4 is yes means "1"
AND
Response to all 5-9 questions is "0"
Epilepsy
Response to ALL questions 2, 3 and 4 is "1" AND response to ALL of the questions 5-9 is "0"
AND / OR
Response to either/both of the questions 10 or 11 is 1
Case Vignette
- 5 year boy came with multiple episodes of sudden vacant stare with unresponsiveness lasted for very few seconds.
- Sometimes during eating or even talking
- No post event confusion or loss of consciousness present
- Frequency near 50-60 episodes/day
- Birth and developmental history were normal. There was no family history of seizures
- He is not taking any medication
INDT-EPI TOOL
Question 1: Has your child ever had fits / daurae / mirgee / chamki?
1.(Yes)
Question 2: Did your child ever have episodes of loss of consciousness associated with any of the following?
- Up rolling of eyes
- Deviation of eyes to one side
- Tongue bite
- Frothing from mouth
- Passing urine / stool in clothes
- Shaking of limbs
- Limbs becoming stiff
0.(N0)
Question 10: Does your child have/had frequent episodes of "going blank" or lose awareness of his/her surroundings?
1.(YES)
Question 11: Did your child ever have ANY of the following without loss of consciousness?(Excluding occasional jerks occurring ONLY during sleep)
0(NO)
Final Diagnosis
Conclusion: Answer to question 10 is yes means "1"
Epilepsy
Response to ALL questions 2, 3 and 4 is "1" AND response to ALL of the questions 5-9 is "0"
AND / OR
Response to either/both of the questions 10 or 11 is 1
Case Vignette
- 3 year old boy visited emergency with history of cough and coryza with fever since last 1 day
- Patient had history of uprolling of eyes with stiffness of all four limbs with loss of unconsciousness and frothing from mouth in early morning during spike of fever. Duration -10 minutes
- History of similar 2 episodes associated with fever lasted for 3-5 minures at 16 months and 30 months of age
- Birth history, developmental history and immunization history was normal
- Child's grandfather had history of similar episodes with fever in his early childhood.
INDT-EPI TOOL
Final Diagnosis
Case Vignette
- 2 year old boy
- Had history of occurrence of unprovoked uprolling of eyes with stiffness of all four limbs with loss of unconsciousness and frothing from mouth 10 days back
- No history of fever at time of seizure
- Duration - 5 minutes
- First episode
- Child was started on oral phenytoin by nearby doctor
- Birth history, developmental history and immunization history was normal
- Family History was normal
INDT-EPI TOOL
Diagnosis ?
Modified INDT Tool for Epilepsy
- Why Modified tool?
- To broaden the age group 0-18 years
- Based on practical definition of epilepsy by ILAE in 2014
- Include description of neonatal seizures
Modified Tool
Yncope