Objectives of The Module
- Overview on autism spectrum disorder
- Describe the core symptoms of Autism Spectrum Disorder (ASD)
- Various evaluation tools for ASD
- Description of INDT-ASD tool
- Clinically evaluate a child with ASD using DSM-IV TR criteria using INDT-ASD tool
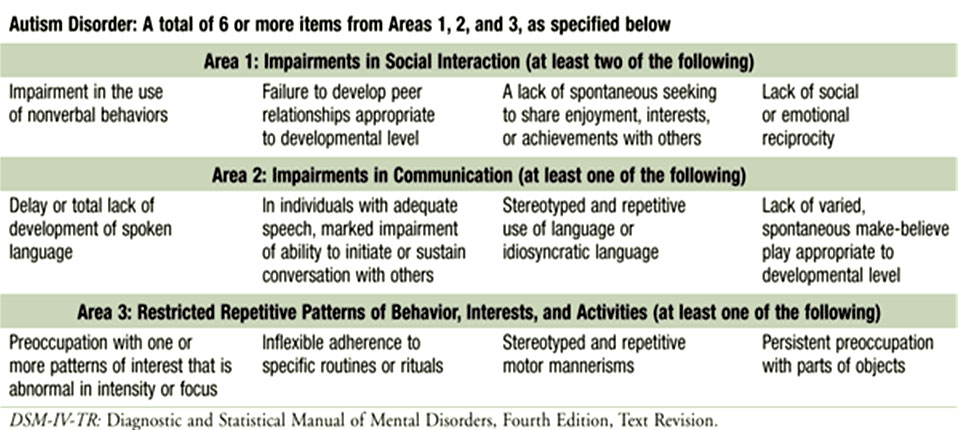
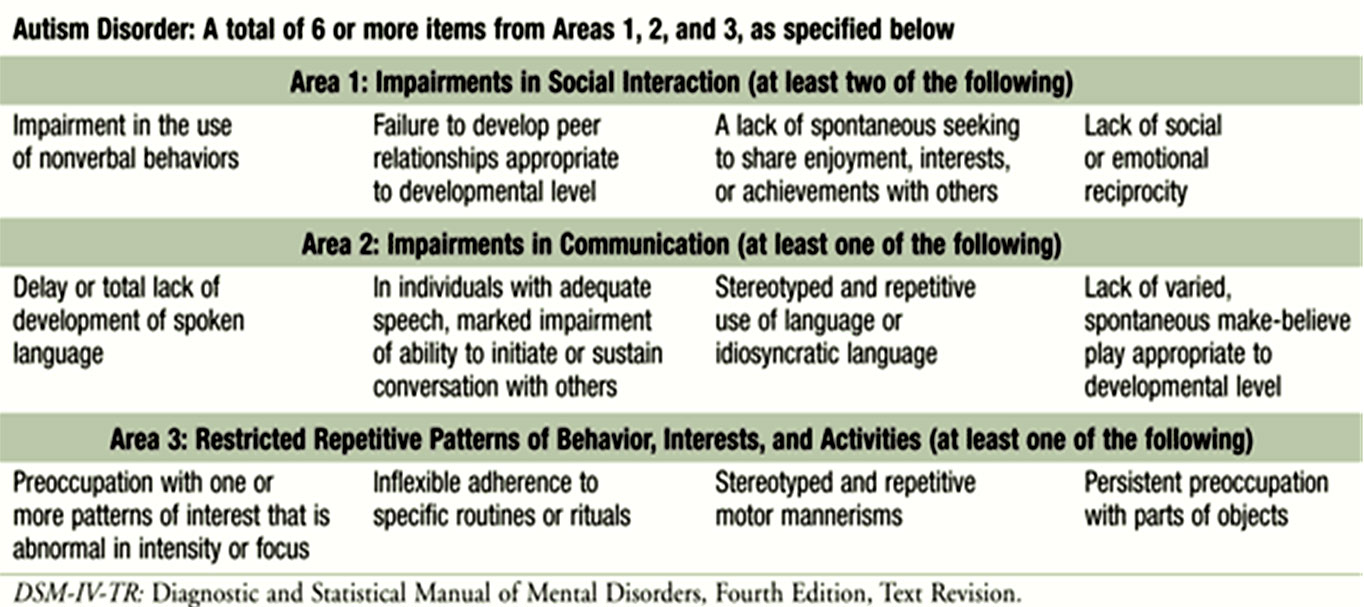
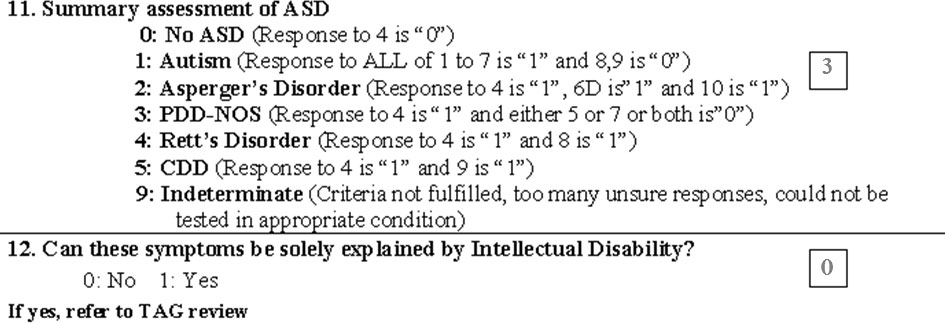
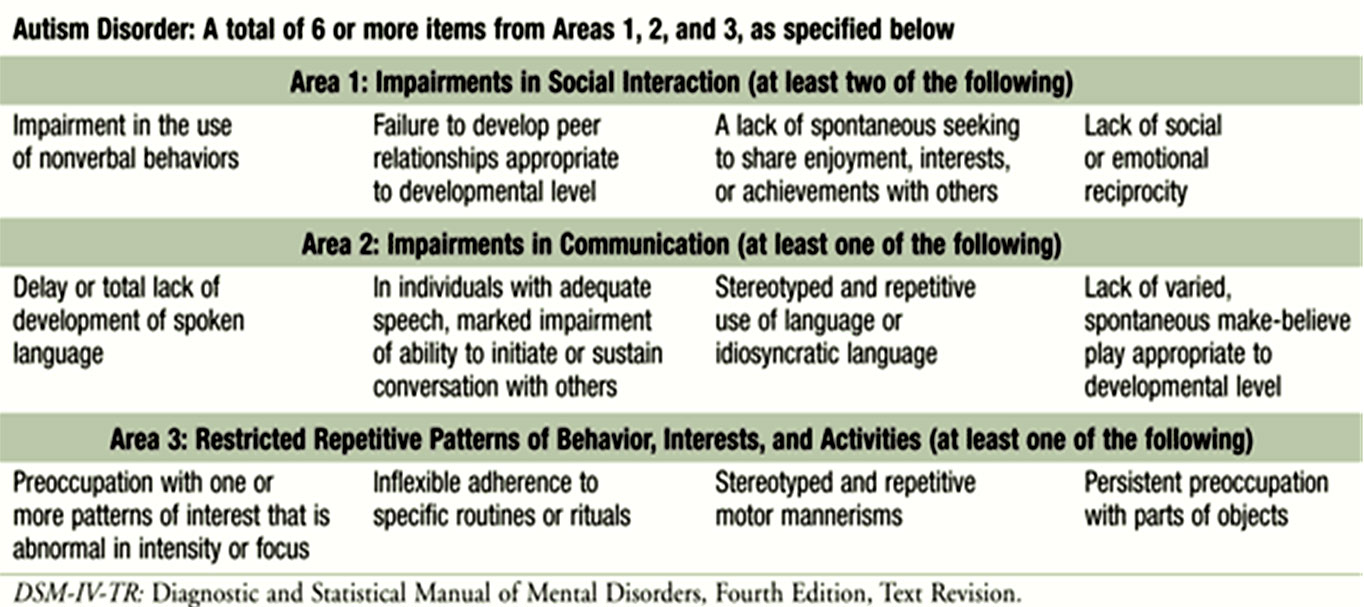
DSM-IV Criteria for Autistic Disorder
- Qualitative impairments in social interaction (2 out of 4 item)
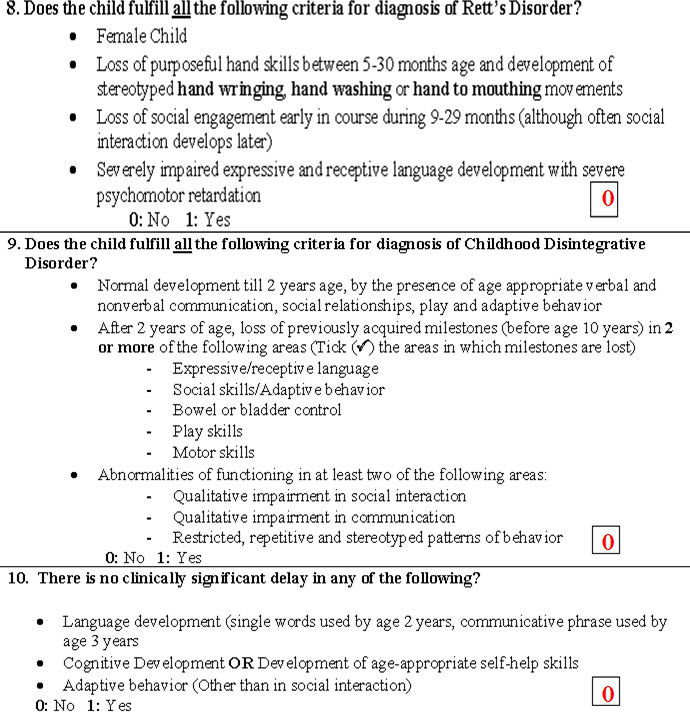
- Qualitative impairments in communication (1 out of 4 items)
- Restricted repetitive and stereotyped patterns of behaviour, interests and activities (1 out of 4 items)
A total of 6 out of 12 items will be called autistic disorder
DSM-IV
Table 2. DSM-IV-TR Criteria for Autistic Disorder
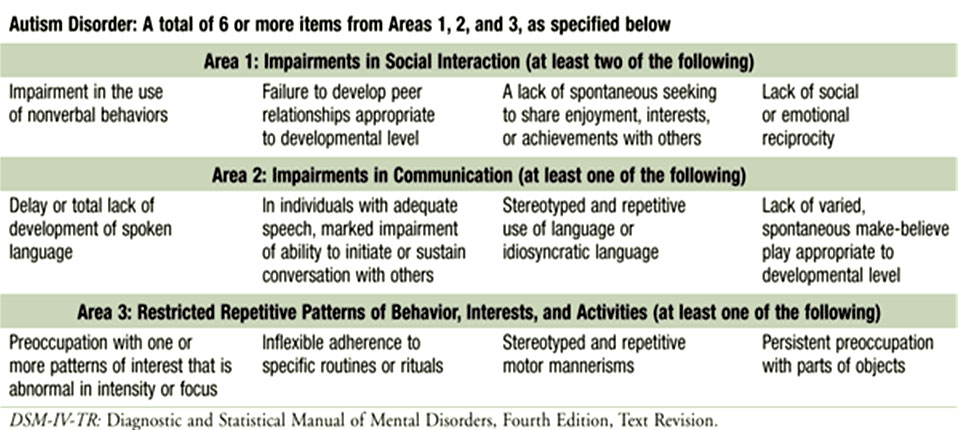
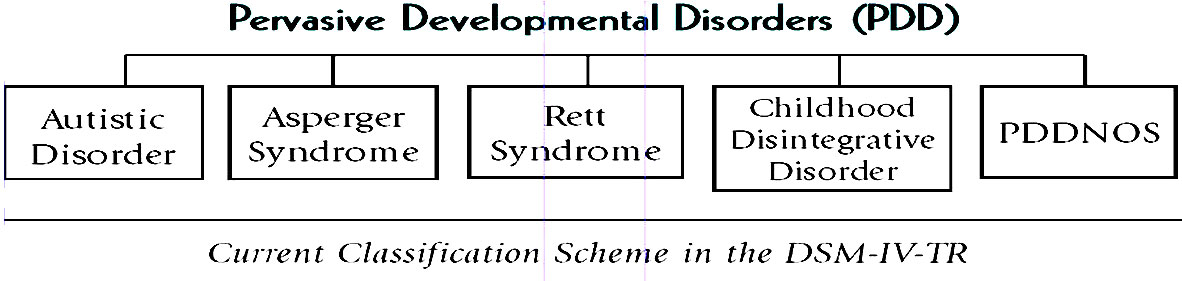
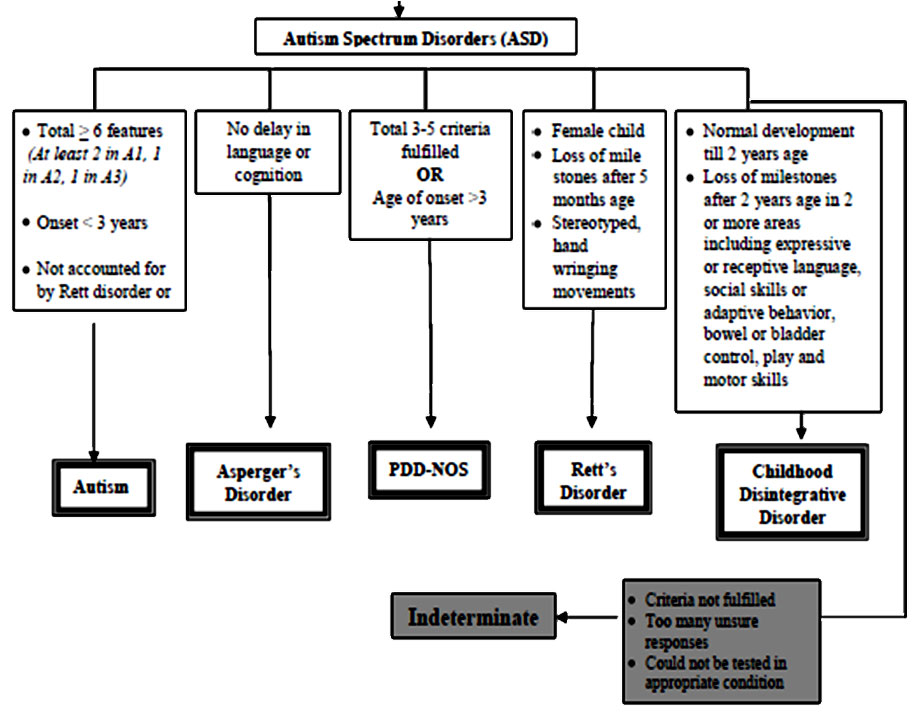
Autism Spectrum Disorders (ASD)
- Autistic disorder/autism
- Asperger’s Syndrome
- Rett’s Disorder
- Childhood Disintegrative Disorder
- Pervasive Developmental Disorder-Not Otherwise Specified (PDD– NOS)
Deficits in Social Interaction
- Impairment in the non-verbal behaviors used for social interaction
- Eye-to-eye contact
- Facial expressions
- Body postures and gestures
- Child may appear to be “in his/her own world”
- Lack of spontaneous sharing of enjoyment and interests with other people
Poor Eye Contact
Legend: The child has a poor eye contact with the examiner
Deficits in Social Interaction
- Social interaction is rarely initiated spontaneously
- Signs of attachment with familiar people or even clinginess to a specific caregiver, or
- Excessive familiarity with strangers due to the absence of social inhibitions and stranger anxiety
- Failure to develop peer relationships appropriate to developmental level
- Lack of spontaneous seeking to share enjoyment, interests, or achievements with other people
- Lack of showing objects of interest to others
- Lack of bringing objects of interest to others
- Lack of pointing out objects of interest
Lack of social or emotional reciprocity
- Not actively participating in simple social play or games
- Preferring solitary activities
- Involving others in activities only as tools or "mechanical" aids
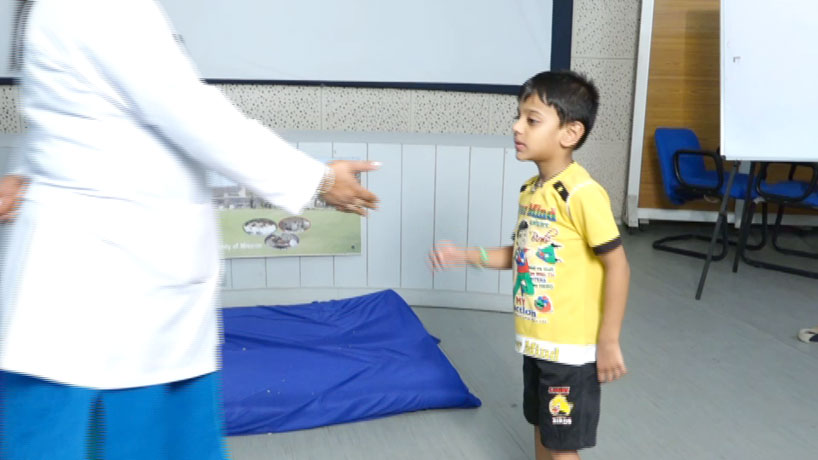
Into Self World

Legend: Child is observed to be not interacting with the examiner and is 'into his own world'
Deficits in Communication
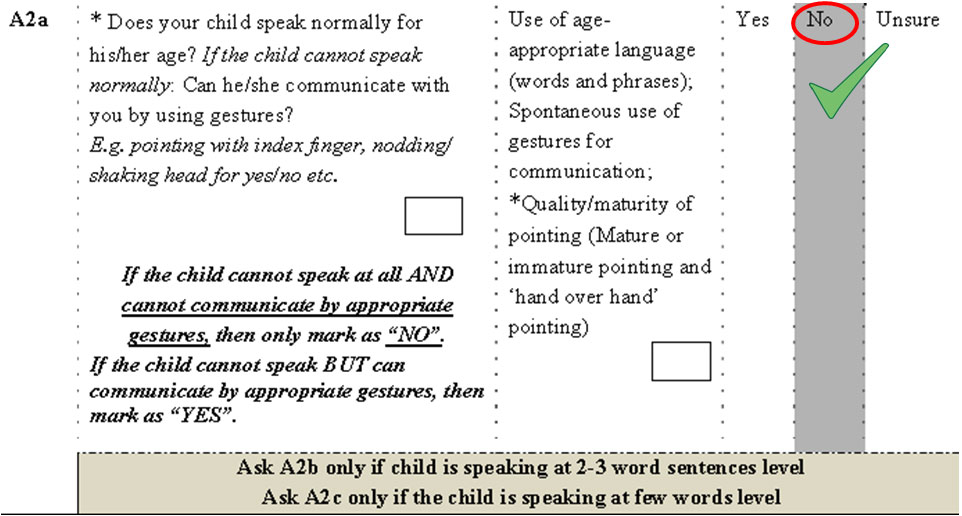
- Deficits in verbal and non-verbal communication
- Delay in or total lack of the development of spoken language (verbal) in absence of attempt to compensate by gestures (non verbal)
- 50% never develop speech
- In the remaining 50%, language acquisition is delayed and/or deviant
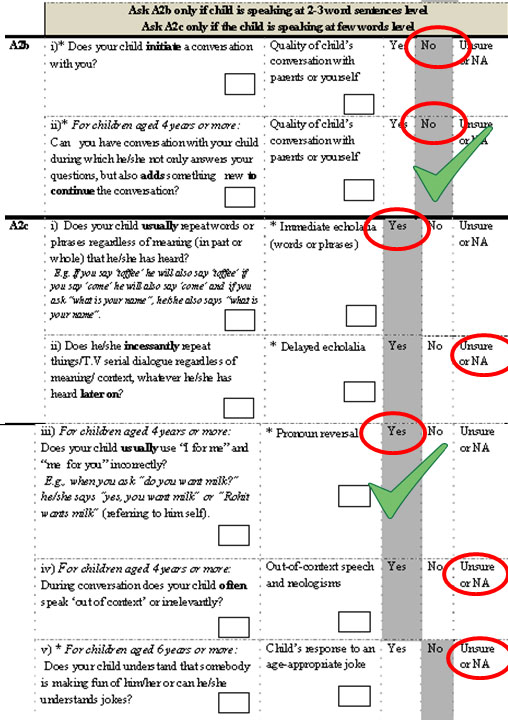
- Impairment in the ability to initiate or sustain a conversation
- Stereotyped, repetitive use of language
- Repetition of words or phrases regardless of meaning or relevance (echolalia)
- Pronominal reversal (substituting ‘I’ for “you’ or vice-versa)
- May not be able to understand gestures or use them during communication
- Lack of social imitative play
- Delayed / absent protodeclarative pointing
Echolalia

Legend: She is observed to repeat the same question asked by the examiner rather than answering it suggestive of echolalia
Restricted and Repetitive Behavior
- Stereotyped and restricted patterns of interest that is abnormal either in intensity or focus
- Inflexible adherence to specific, non-functional routines or rituals
- Stereotyped and repetitive motor mannerisms
- Hand or finger flapping
- Body twisting
- Complex whole-body movements
- Preoccupation with parts of objects
Motor Stereotypies

Child is observed to have motor stereotypies in the form of bouncing, hand flapping movements, and is also seen to be preoccupied with thread and in his own world
Motor Stereotypies

Spinning objects
Other Features in Autism
- Sensory symptoms: Visual, auditory, olfactory, perceptual, and increased sensitivity to touch
- Play: Atypical or deviant, mechanical and repetitive, Lining things up
- Abnormalities of mood or affect
Inappropriate to the situation or circumstances
- Inappropriate fear
Oblivious to hazards or may have excessive fear of harmless objects
Asperger Disorder
- Marked difficulties in socialization
- One-sided communication style
- Rigid pattern of interests focused on rote memorization of factual information
- Paucity of nonverbal communication
- Lack of empathy
- Tendency to intellectualize emotions
- Motor clumsiness
- Preserved intellectual skills
Rett's Disorder: Phases
- Phase I: Normal development for the first 5-18 months of life
- Phase II: Slowing of acquisition of developmental milestones
- Phase III: Rapid deterioration with loss of previously acquired speech, and lack of interest in social relationships.
- Loss of purposeful hand movements with "hand washing and wringing" movements develop
- Phase IV: Social skills may improve later in life
Features
- Intellectual disability
- Acquired microcephaly
- Both in girls and in males who have mutations of MECP2
- Breathing irregularities
- Cardiac arrhythmias.
Childhood Disintegrative Disorder (CDD) or Heller's Disease
- Normal development until 2-3 years age.
- Followed by regression of bowel and bladder training, language and social skills
- May also develop autistic-like stereotypies
- Regression may plateau or continue to be progressive
Childhood Disintegrative Disorder (CDD) or Heller's Disease
- Normal development until 2-3 years age.
- Followed by regression of bowel and bladder training, language and social skills
- May also develop autistic-like stereotypies
- Regression may plateau or continue to be progressive
Pervasive Developmental Disorder – Not Otherwise Specified (PDD-NOS)/ "atypical autism"
- Criteria are not fulfilled for a specific ASD presentations
One or all of following:
- Late age at onset
- Atypical symptomatology
- Sub threshold symptomatology
Co–morbidity
- Psychiatric Disorders
- Intellectual Disabilities
- Epilepsy / Seizures
- Feeding Distrubances and Gastrointestinal problems
- Sleep Disturbances
Natural History
- Infancy: Delayed language development.
- Clinical spectrum changes with age and level of developmental maturity.
- Deficits continue into and through adult life
- Social behavior remains deviant
- Hyperactivity tends to improve and ritualistic behaviors start decreasing during adolescence
- Depression may develop in some high functioning autistic individuals
Research Paper
INCLEN Diagnostic Tool for Autism Spectrum Disorder (INDT-ASD): Development and Validation
- The diagnostic accuracy [AUC=0.97 (0.93, 0.99); P<0.001]
- Sensitivity 98%, specificity 95%, PPV 91%, NPV 99%
- Concordance rate between the INDT-ASD and expert diagnosis for ‘ASD group’ was 82.52% [Cohen’s κ=0.89; 95% CI (0.82, 0.97); P=0.001]
- The convergent validity with CARS (r = 0.73, P= 0.001)
Indian Pediatr 2014; 51: 359-65
Consensus Clinical Criteria (CCC)
- The criteria for diagnosis is based on best currently available evidence and / or consensus among national and international experts, using minimal investigations to serve the needs of resource-constrained settings
- Questionnaires and direct observation (both structured and unstructured settings)
- Based on DSM-IV TR criteria
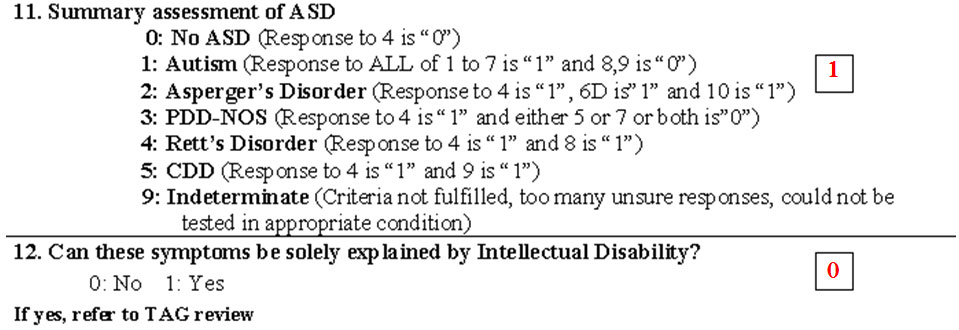
INDT-ASD Diagnostic Tool for ASD
- Merits:
- High diagnostic accuracy
- Adequate content validity
- Good internal consistency
- Easy to administer; no training required
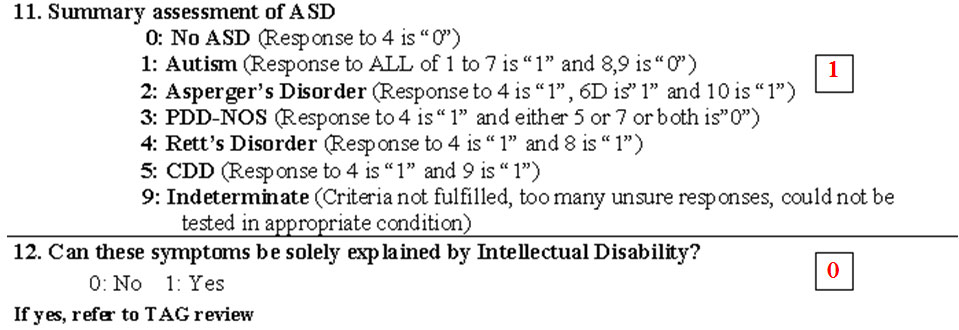
DSM-IV Criteria for Autism
- Qualitative impairment in social interaction
(2 out of 4 item)
- Qualitative impairments in communication
(1 out of 4 items)
- Restricted repetitive and stereotyped patterns of behaviour, interests and activities (1 out of 4 items)
A total of 6 out of 12 items will be called autistic disorder
DSM- IV TR Criteria for Autism
- Total of six (or more) items from (1), (2), and (3)
- At least two from section (1)
- At least one each from (2) and (3)
DSM-IV
Table 2. DSM-IV-TR Criteria for Autisitc Disorder
Qualitative Impairment in Social Interaction (Section 1)
- Marked impairment in the use of multiple nonverbal behaviors such as eye-to-eye gaze, facial Expression, body postures, and gestures to regulate social interaction.
- Failure to develop peer relations appropriate to developmental level
- A lack of spontaneous seeking to share enjoyment, interests, or achievements with other people (e.g. by a lack of showing, bringing, or pointing out objects of interest)
- Lack of social or emotional reciprocity (give-and-take)
Impairment in Communication (Section 2)
- Delay in, or total lack of, the development of spoken language (not accompanied by an attempt to compensate through alternative modes of communication such as gesture or mime)
- In individuals with adequate speech, marked impairment in the ability to initiate or sustain a conversation with others
- Stereotyped and repetitive use of language
- Lack of varied, spontaneous make-believe play or social imitative play appropriate to developmental level
Restrictive Repetitive and Stereotyped Pattern of Behavior,
Interests and Activities (Section 3)
- Encompassing preoccupation with one or more stereotyped and restricted patterns of interest that is abnormal either in intensity or focus
- Apparently inflexible adherence to specific, nonfunctional routines or rituals
- Stereotyped and repetitive motor mannerism (e.g., hand or finger flapping or twisting, or complex whole-body movements)
- Persistent preoccupation with parts of object
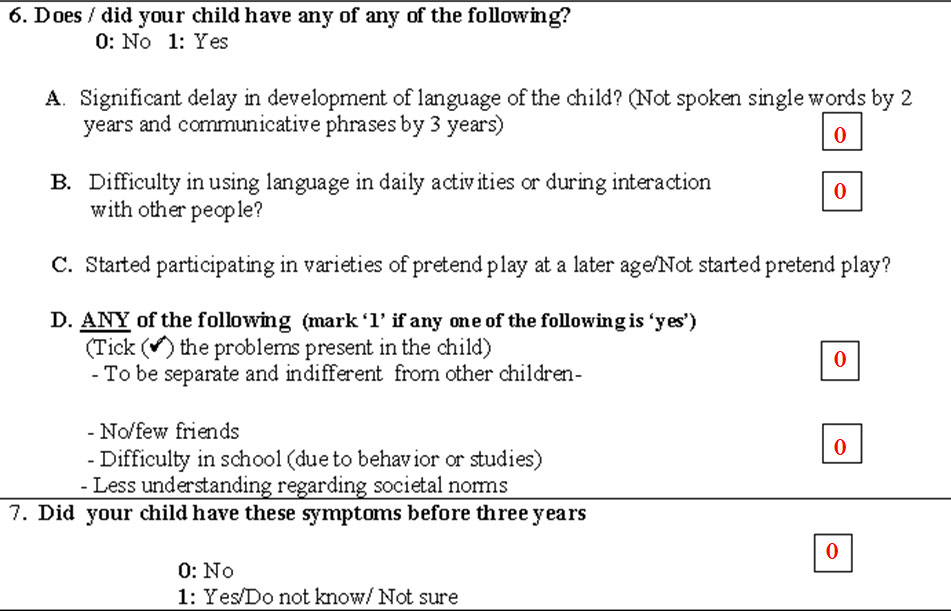
Additional Criteria for Autism
- Delays or abnormal functioning in at least one of the following areas
- Social interaction
- Language as used in social communication
- Symbolic or imaginative play
- Onset prior to age 3 years
- The disturbance is not better accounted for by Rett’s Disorder or Childhood disintegrative disorder
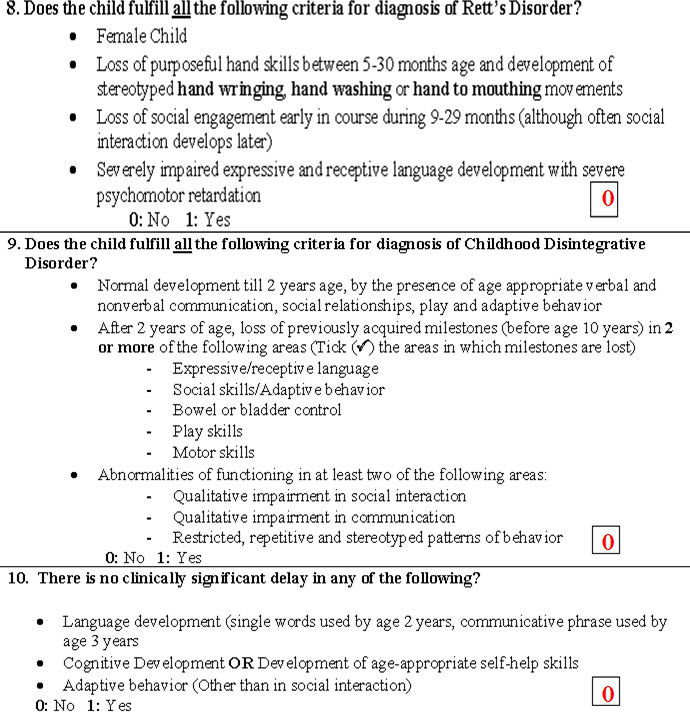
- There is no clinically significant delay in language (e.g., single words used by age 2 years, communicative phrases used by age 3 years)
- There is NO clinically significant delay in cognitive development or in the development of age appropriate self-help skills, adaptive behavior (other than in social interaction), and curiosity about the environment in childhood
- Criteria are not met for another specific pervasive developmental disorder
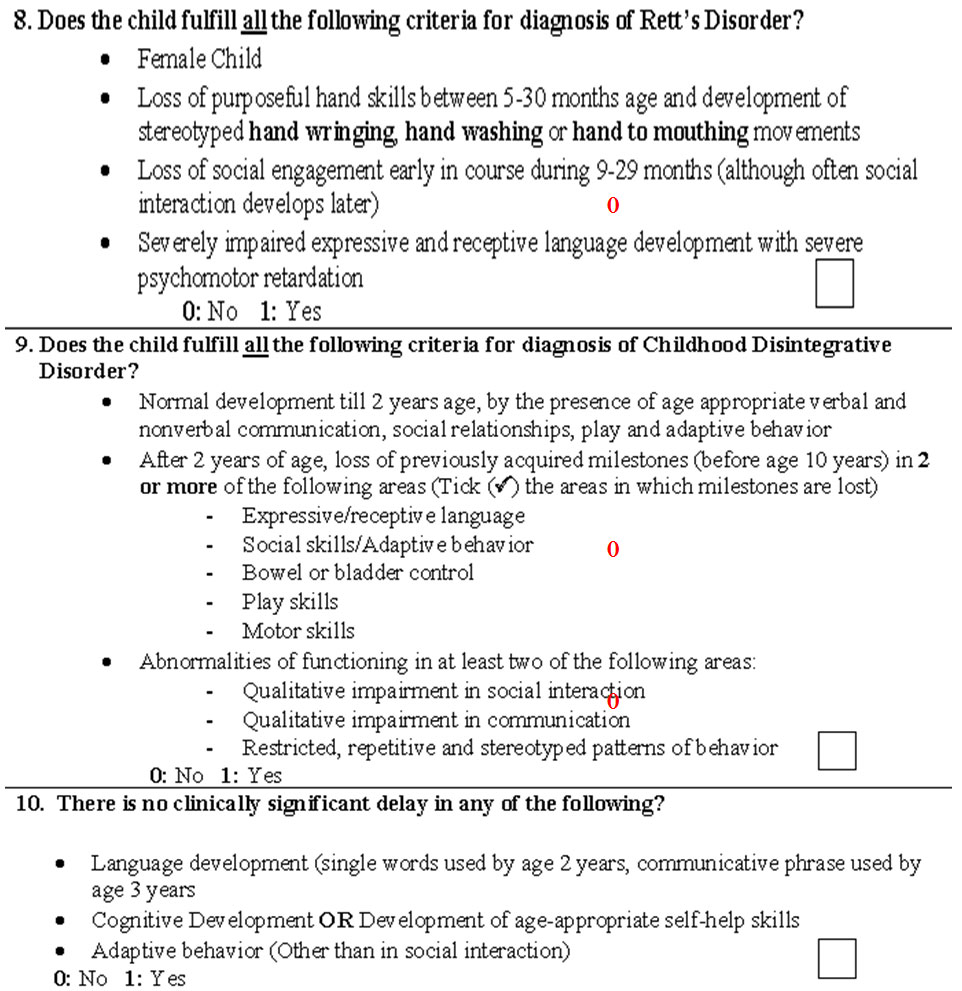
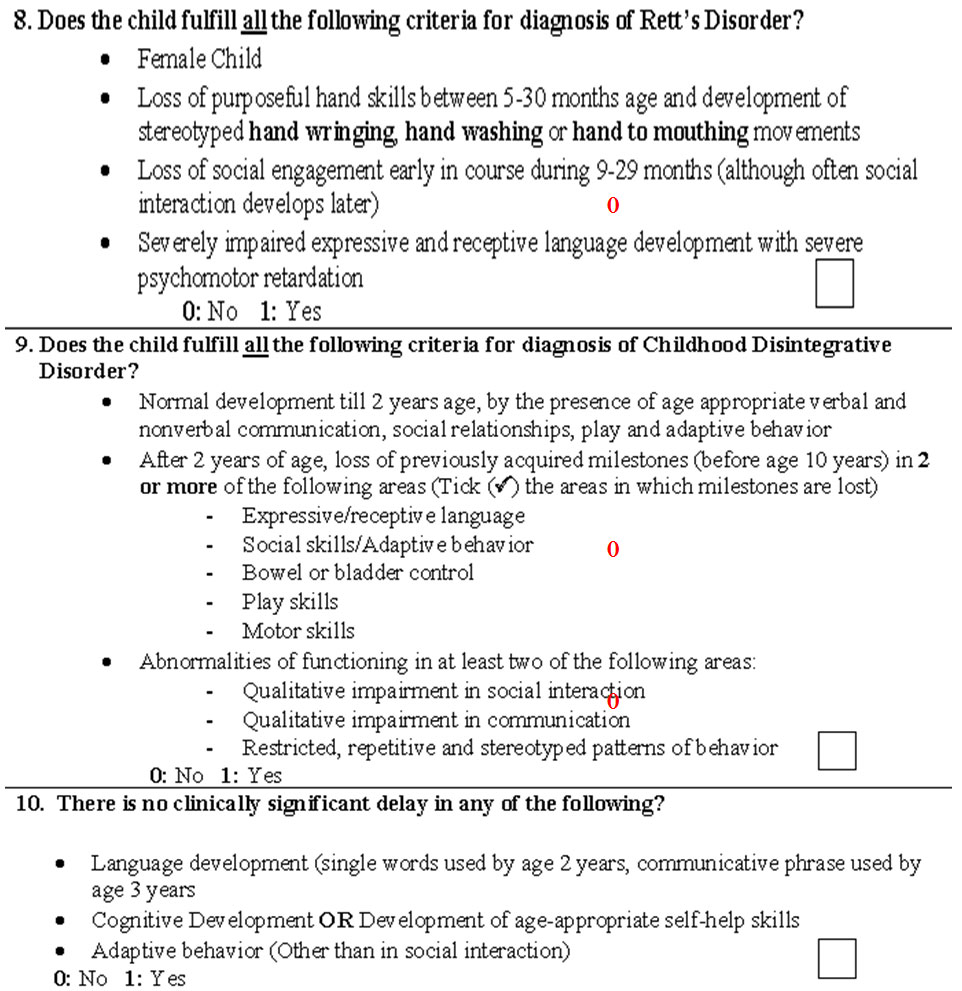
Consensus Criteria for Diagnosis of Rett's Disorder
- Apparently normal prenatal and perinatal development
- Normal psychomotor development through the first five months of life
- Normal head circumference at birth
- There is loss of previously acquired purposeful hand skills between the age of 5 and 30 months
- Subsequent development of stereotyped hand movements (e.g., hand wringing or hand washing)
Consensus Criteria for Diagnosis of Rett's Disorder (DSM-IV TR Criteria)
(A) All of the following:
- Apparently normal prenatal and perinatal development
- Apparently normal psychomotor development through the first five months after birth
- Normal head circumference at birth
(B) Onset of all of the following after the period of normal development:
- Deceleration of head growth between ages 5 and 48 months
- Loss of previously acquired purposeful hand skills between ages 5 and 30 months with the subsequent development of stereotyped hand movements (e.g., hand wringing or hand washing)
- Loss of social engagement early in the course (although often social interaction develops later)
- Appearance of poorly coordinated gait or trunk movements
- Severely impaired expressive and receptive language development with severe psychomotor retardation
Childhood Disintegrative Disorder
- There is marked regression in multiple areas of functioning following a period of at least 2 years of apparently normal development.
- There is clinically significant loss of previously acquired skills (before age 10 years) in at least two of the following areas:
- Expressive or receptive language
- Social skills
- Bowel or bladder control
- Play or motor skills.
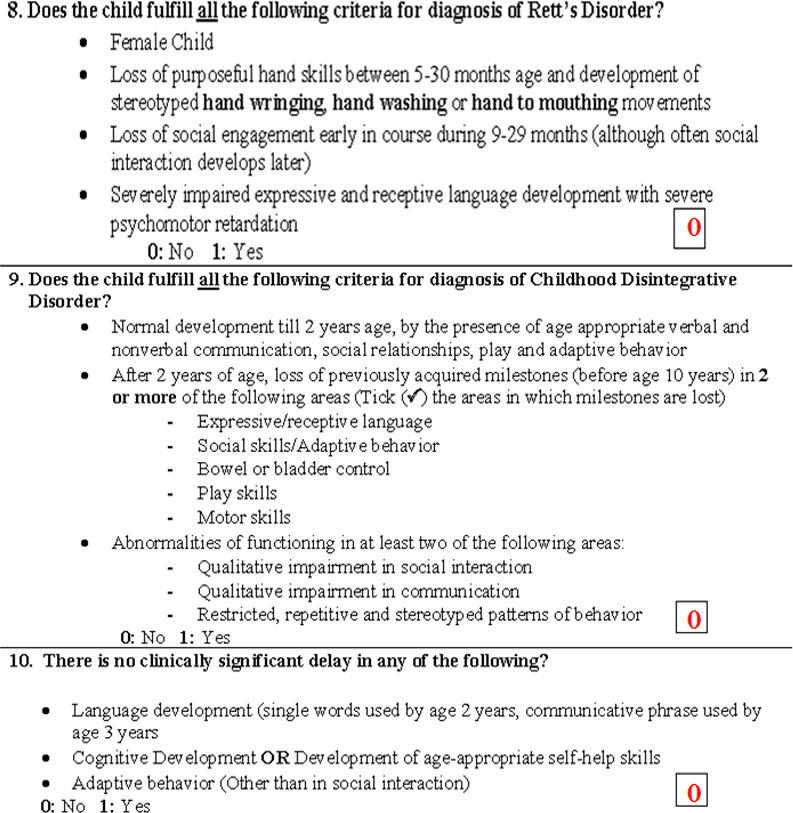
Consensus Criteria for Diagnosis of Childhood Disintegrative Disorder (DSM IV)
A. Apparently normal development for at least the first two years after birth as manifested by the presence of age-appropriate verbal and nonverbal communication, social relationships, play, and adaptive behavior
B. Clinically significant loss of previously acquired skills (before age 10 years) in at least two of the following areas:
- Expressive or receptive language
- Social skills or adaptive behavior
- Bowel or bladder control
- Play
- Motor skills
C. Abnormalities of functioning in at least two of the following areas:
- Qualitative impairment in social interaction (e.g., impairment in nonverbal behaviors, failure to develop peer relationships, lack of social or emotional reciprocity)
- Qualitative impairments in communication (e.g., delay or lack of spoken language, inability to initiate or sustain a conversation, stereotyped and repetitive use of language, lack of varied make-believe play)
- Restricted, repetitive, and stereotyped patterns of behavior, interests, and activities, including motor stereotypies and mannerisms)
Consensus Criteria for Diagnosis of Pervasive Developmental Disorder-NOS (PDD-NOS)
A. Diagnosis of “PDD-NOS” is made in the following conditions:
- When the child fulfils the diagnostic criteria for Autism, but age of onset of symptoms is after 3 years
- When the child has impaired social interaction and either impaired verbal/non-verbal communication or restrictive, repetitive, and stereotyped patterns of behaviors, interests, and activities, but total number of criteria fulfilled is 3-5 (instead of 6)
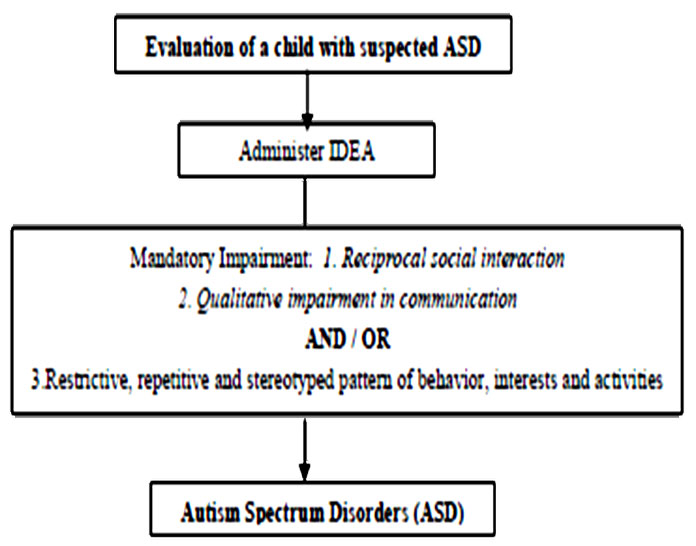
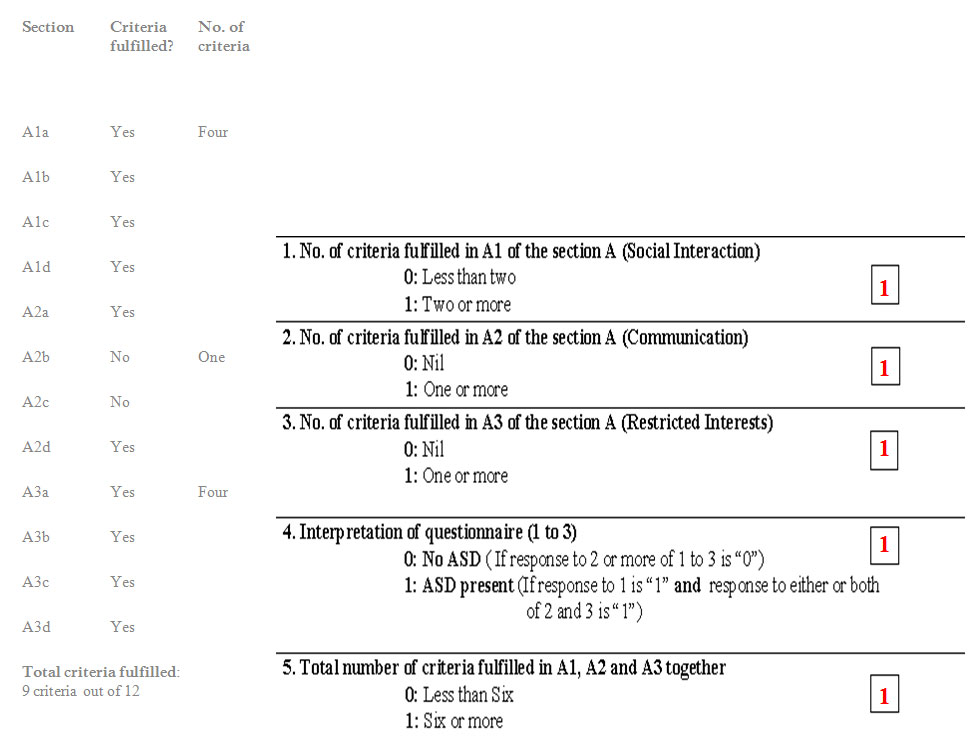
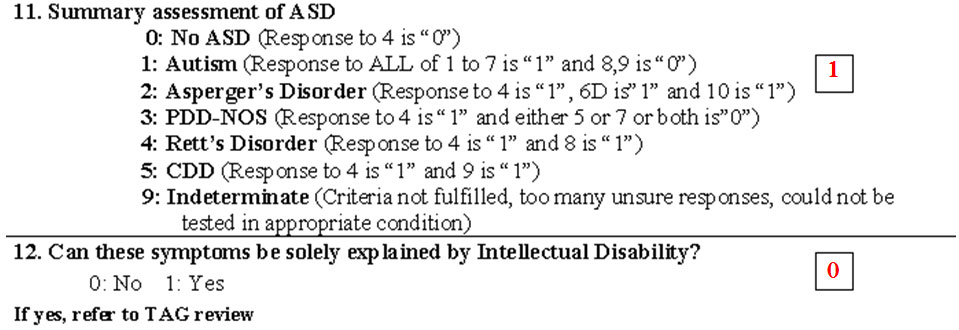
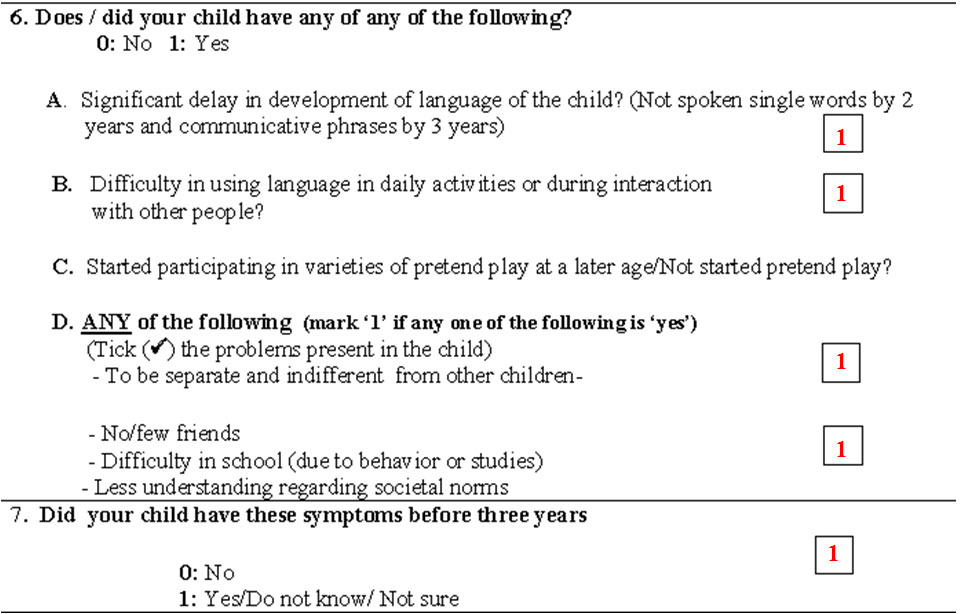
Algorithm for Evaluation of ASD
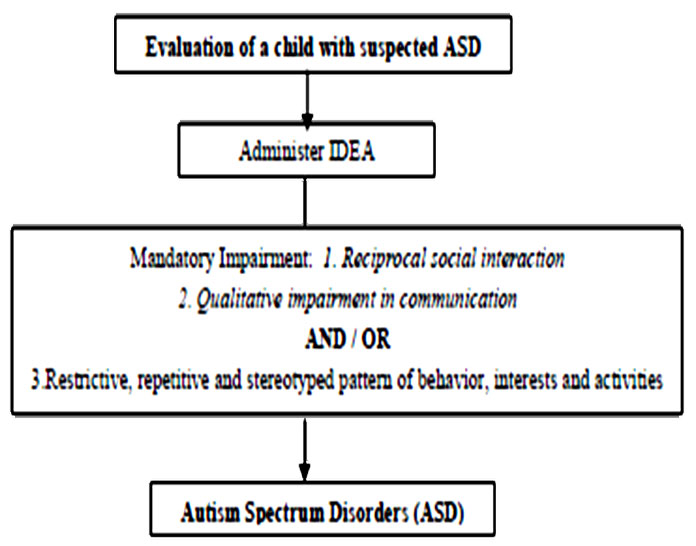
INDT-ASD Diagnostic Tool
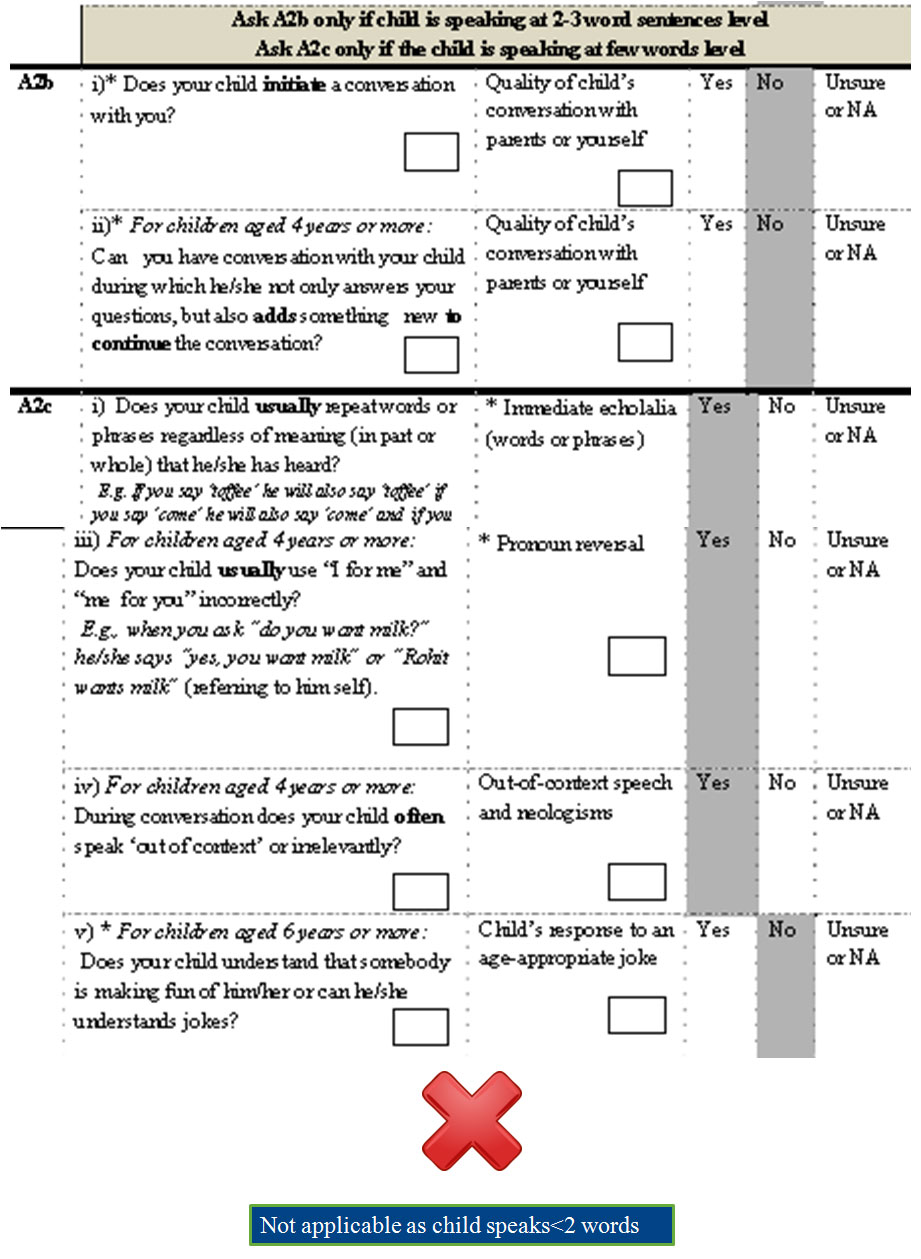
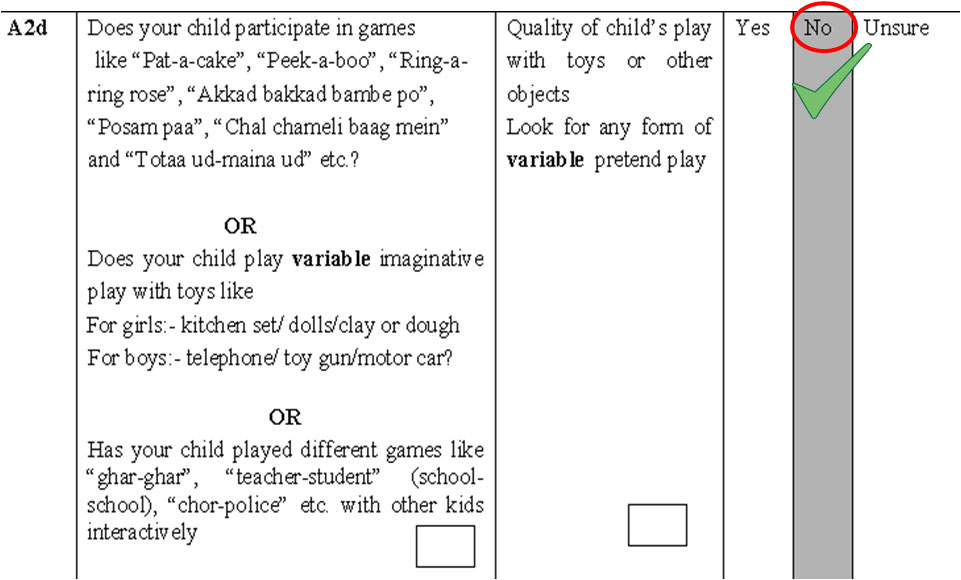
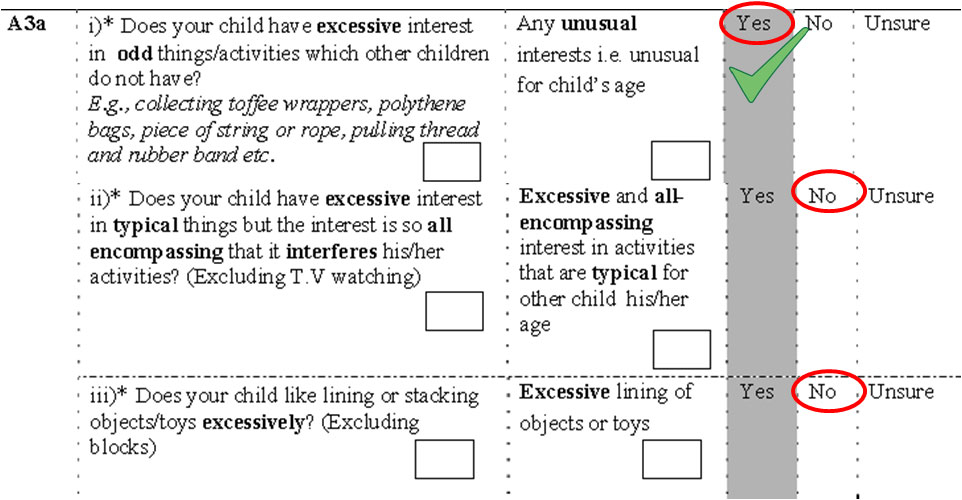
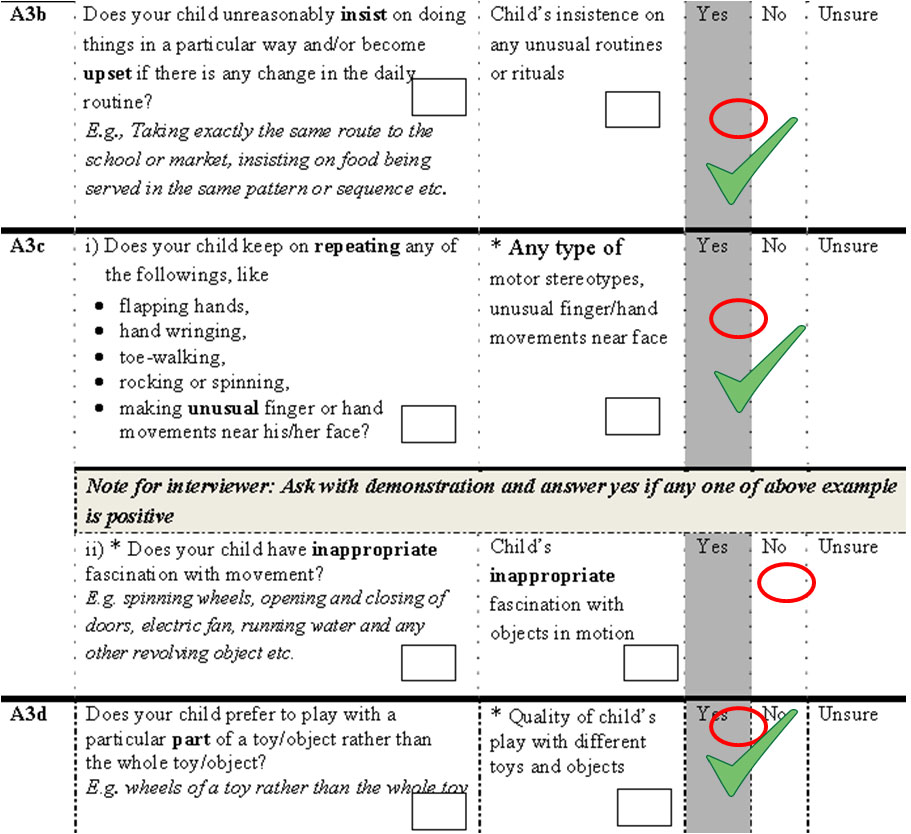
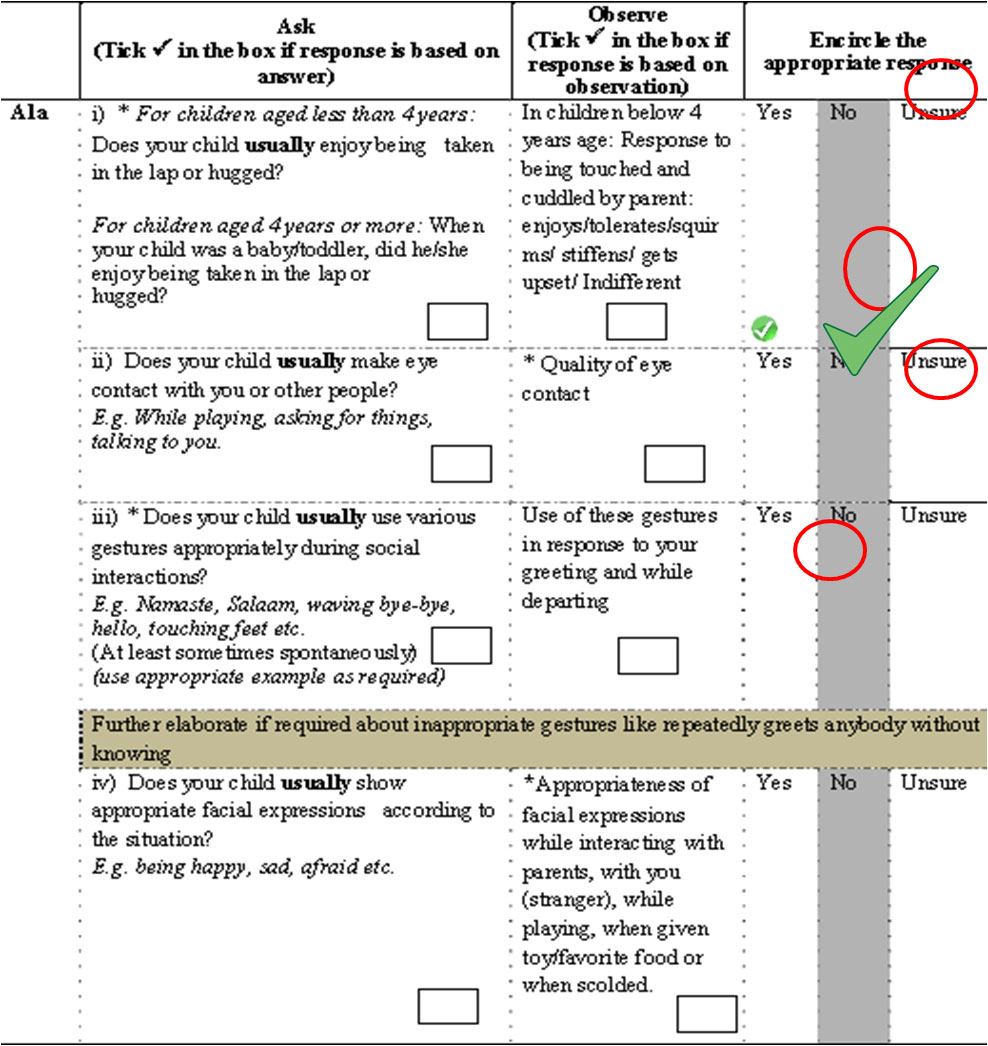
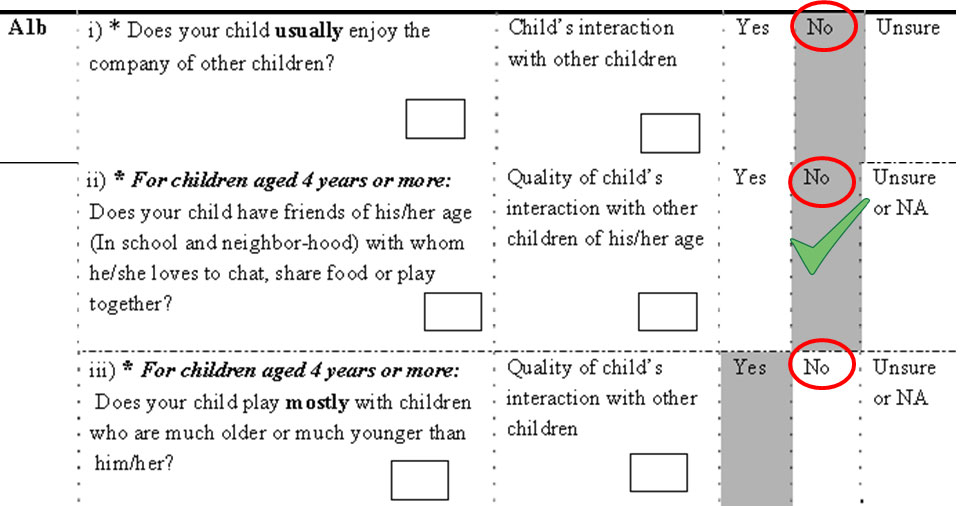
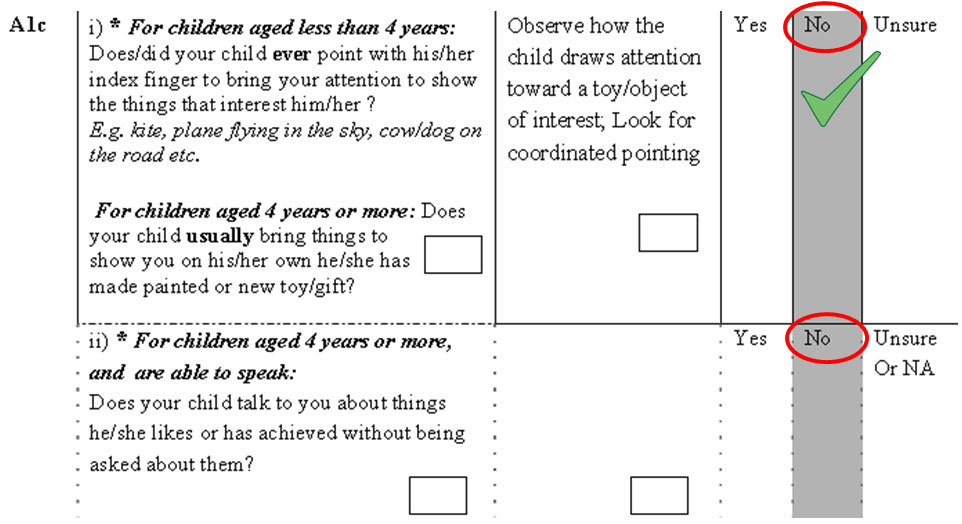
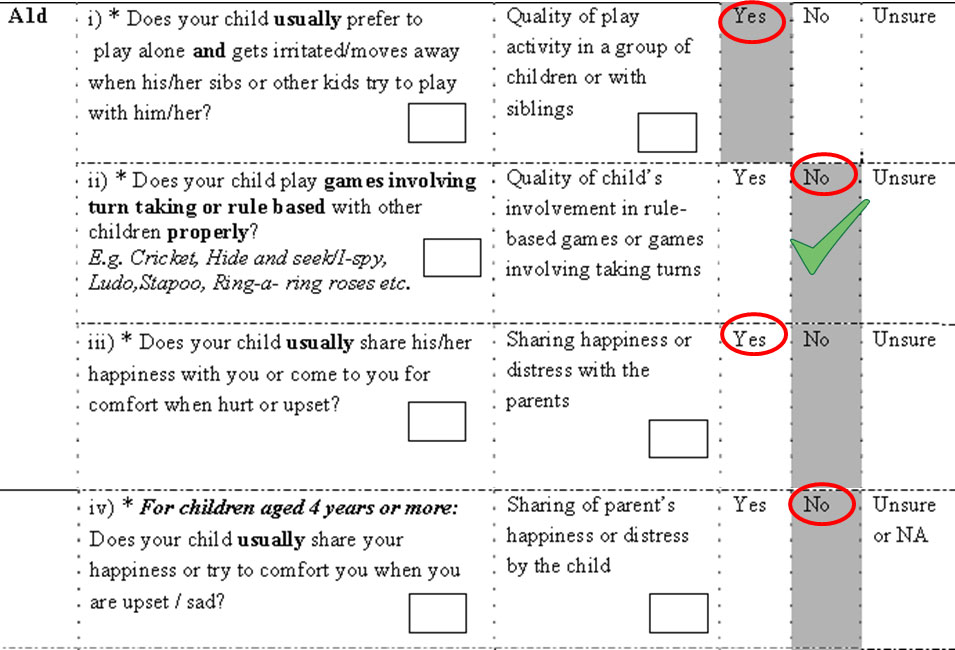
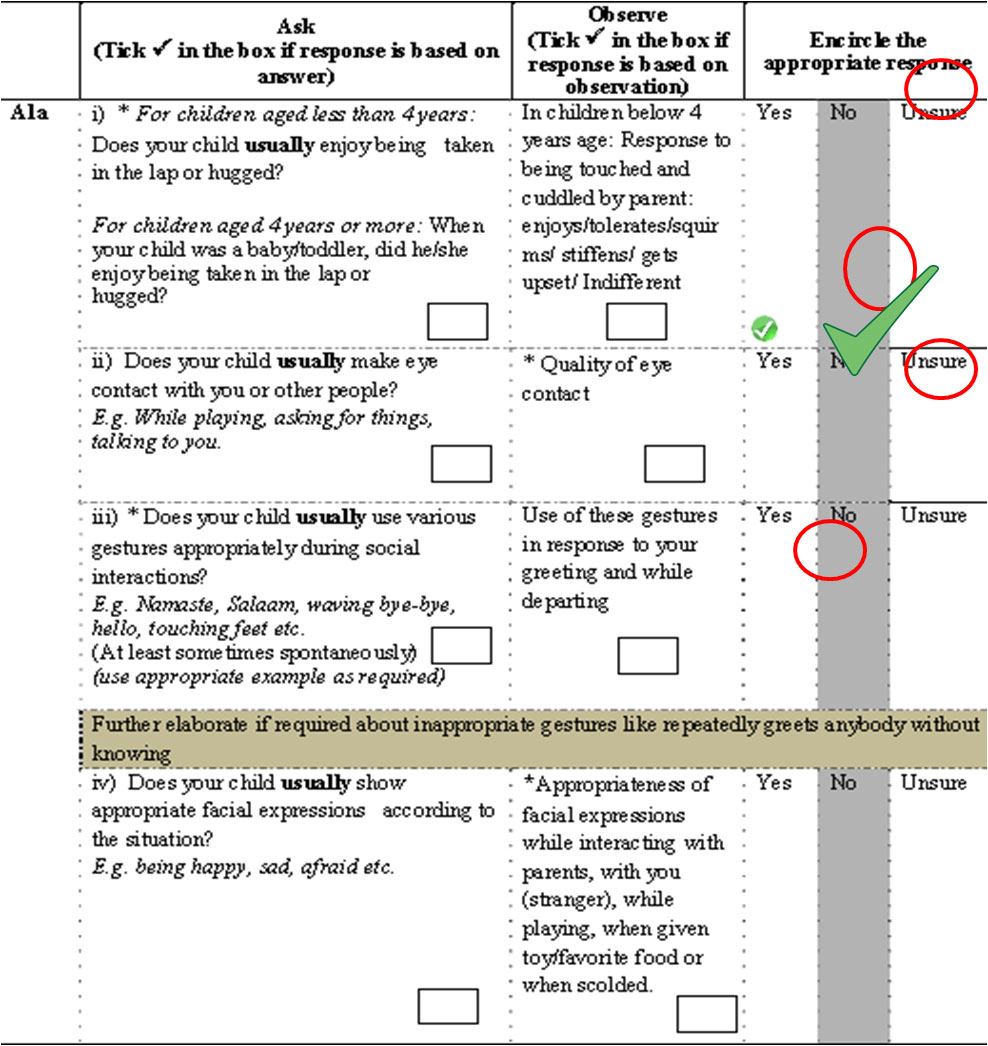
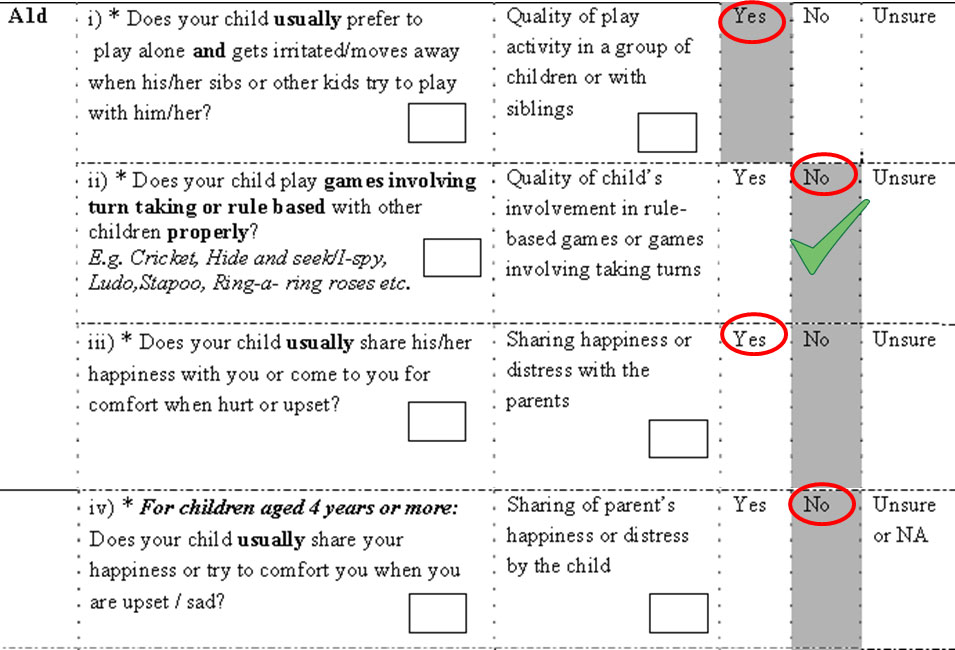
- The tool has two sections:
- Section A has 29 symptoms/items
- Section B contains 12 questions corresponding to B and C domains of DSM-IV-TR, time of onset, duration of symptoms, score and diagnostic algorithm.
- It takes approximately 45-60 minutes to administer the instrument and score.
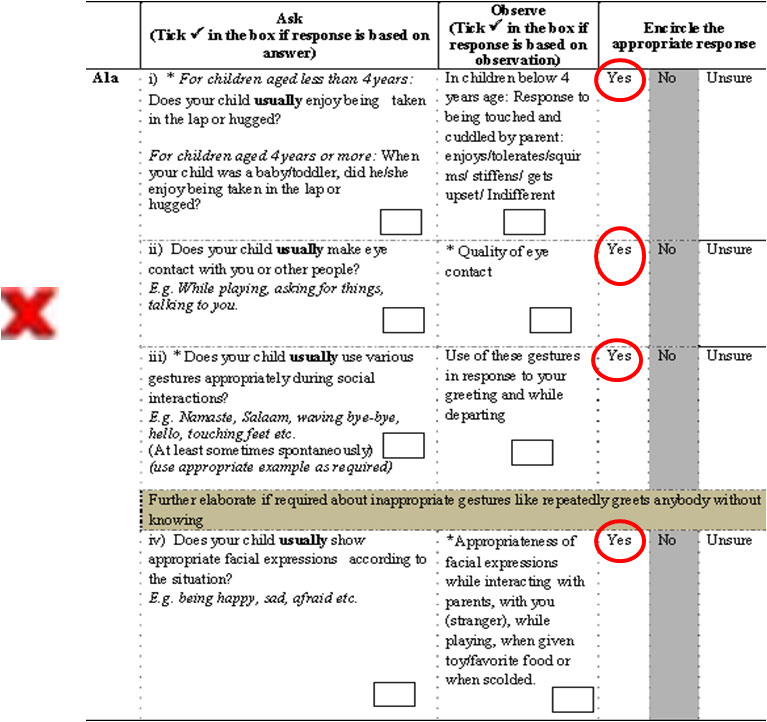
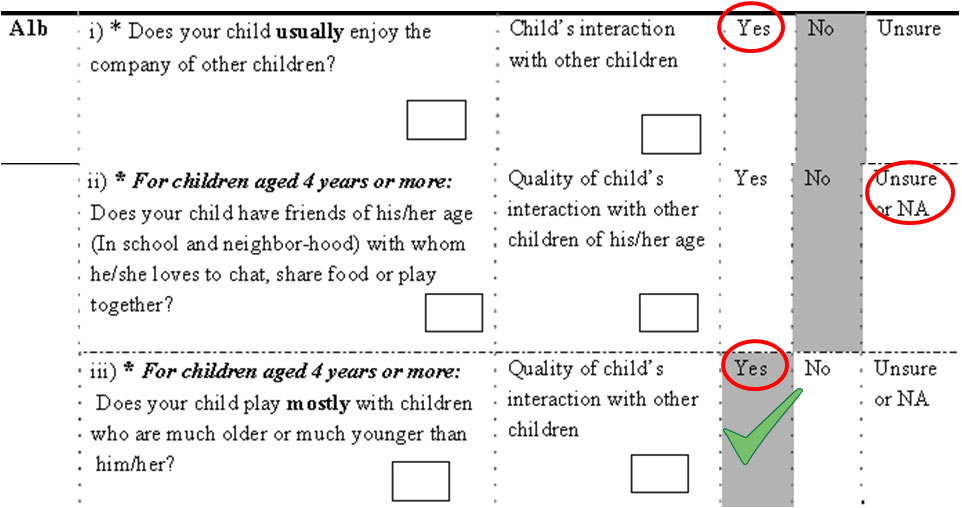
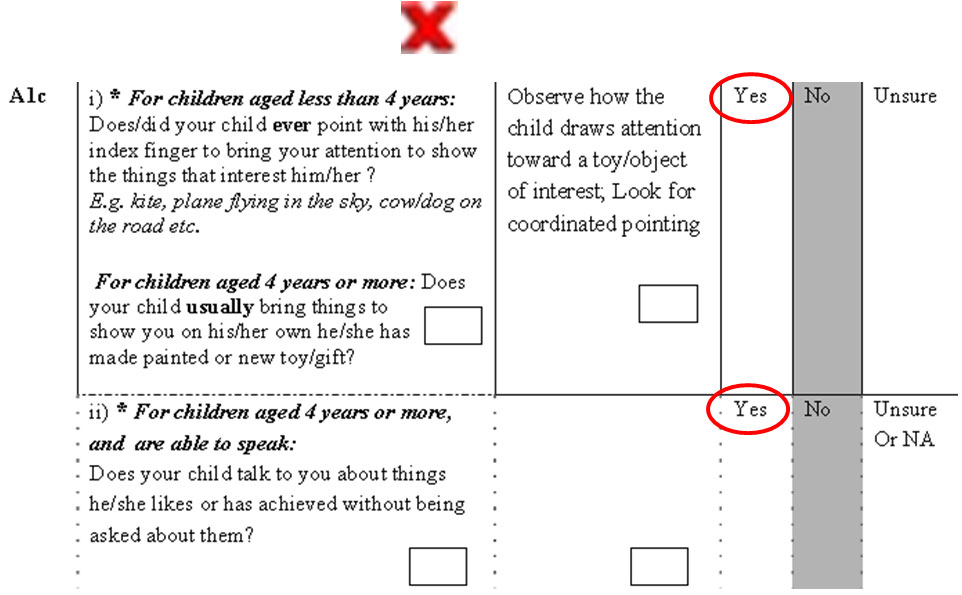
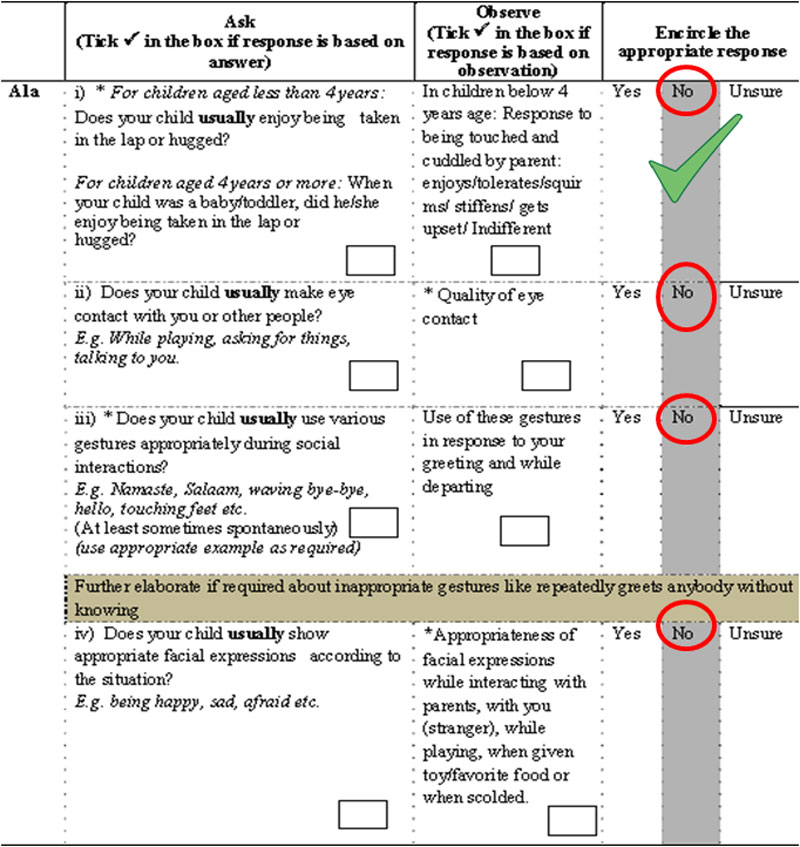
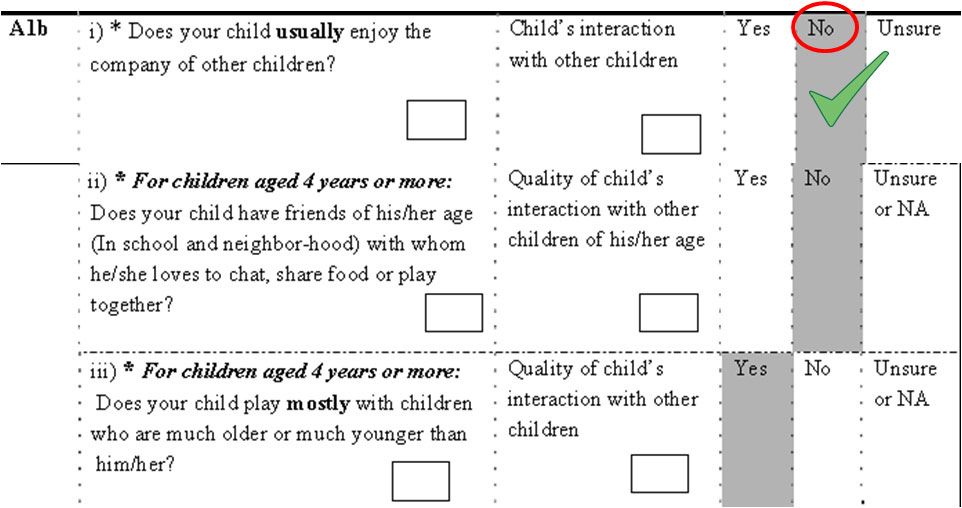
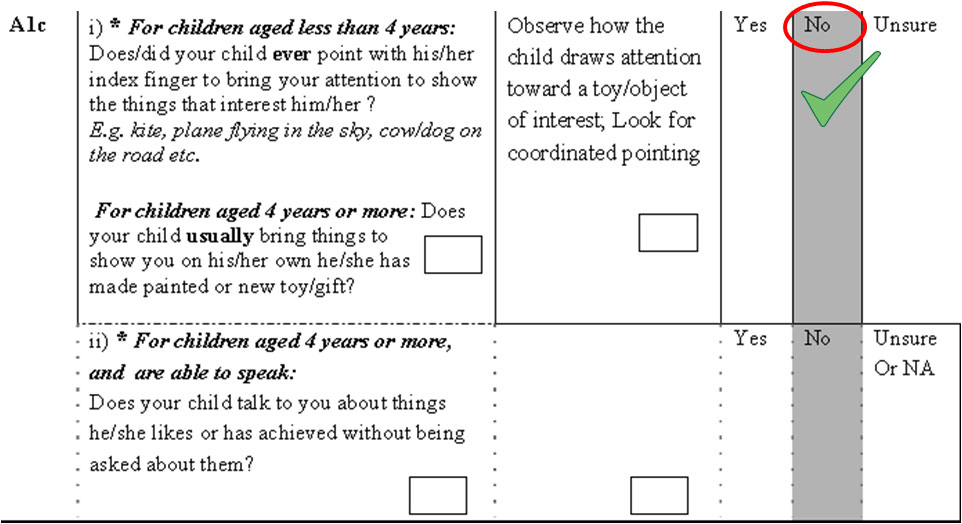
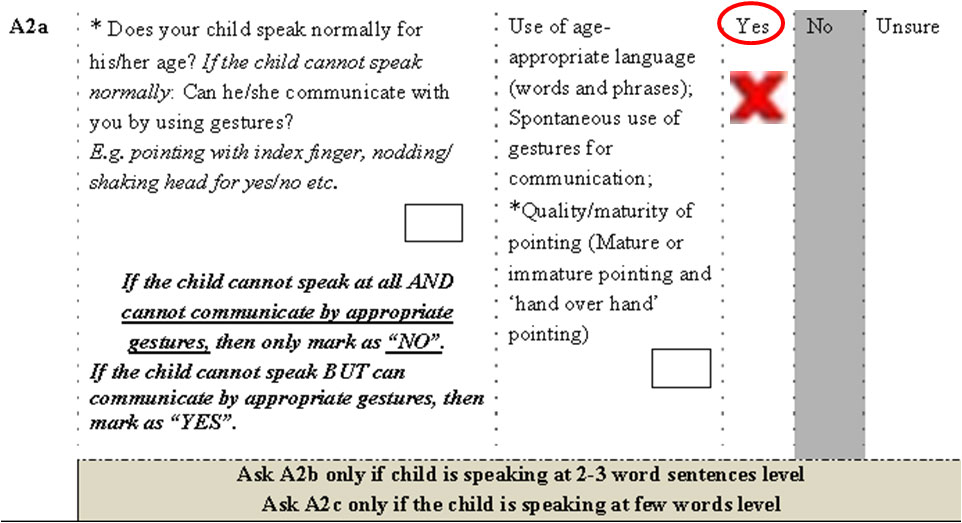
- A trichotomous endorsement choice (‘yes’, ‘no’, ‘unsure/not applicable’) is given to the assessor/ interviewer.
- Clinician/psychologist has to make behavioral observations on the child and score the item as well.
- For any discrepancy in parental response and interviewer’s assessment, it is indicated for each question whether parental response or assessor’s observation should take precedence.
- Each symptom/item is given a score
- ‘1’ for ‘Yes’
- ‘0’ for ‘No’ or ‘unsure/not applicable’.
- Presence of ≥ 6 symptoms/item (or score of ≥ 6), with at least two symptom/item each from impaired communication and restricted repetitive pattern of behavior, is used to diagnose ASD
Instructions For Evaluation
- Primary caregiver must be present with the child
- These behaviors are to be assessed in the context of children of same age
- Explain to parents that the answers should be based on the child’s behavior most of the time
- Follow the age directions given along with the question. For questions where no age cut-off is given, they should be asked for all children i.e. all ages (2-9 years)
- Ask the questions verbatim
- Question can be repeated if the respondent cannot understand
- Still, if the respondent cannot understand, give example for the particular behavior; No further elaboration is allowed
- The questionnaire should be supplemented by observations for the suggestive behavior in the child throughout the assessment.
- Observe the behavior of the child during the entire interview to confirm the presence or absence of a particular behavior (First ask, then observe if observation is discrepant, then re-ask the question and recheck the observation also).
- When there is discrepancy between parental response and your observation, * indicates whether parent report or observation should take precedence, and marked accordingly.
- When parent's response is "Unsure", your observation of the particular behaviour will be given weightage even when asterisk (*) is on parental response. In case your are also unable to observe the behavior, then only mark the response as "Unsure"
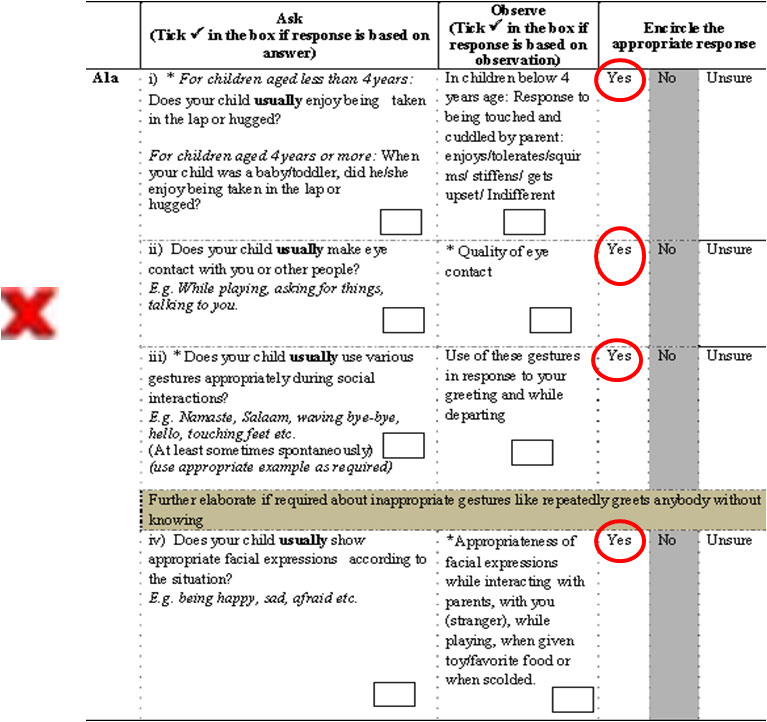
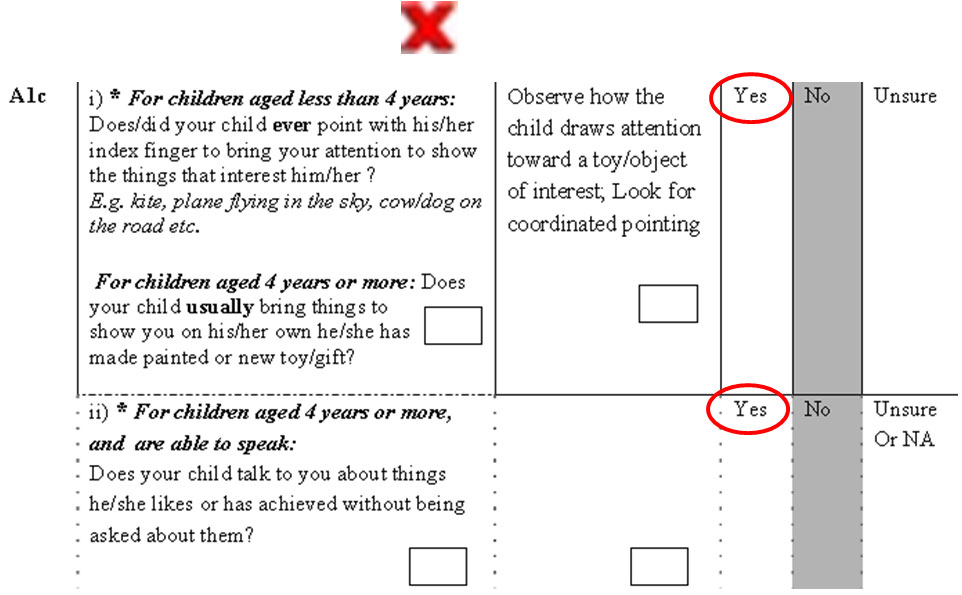
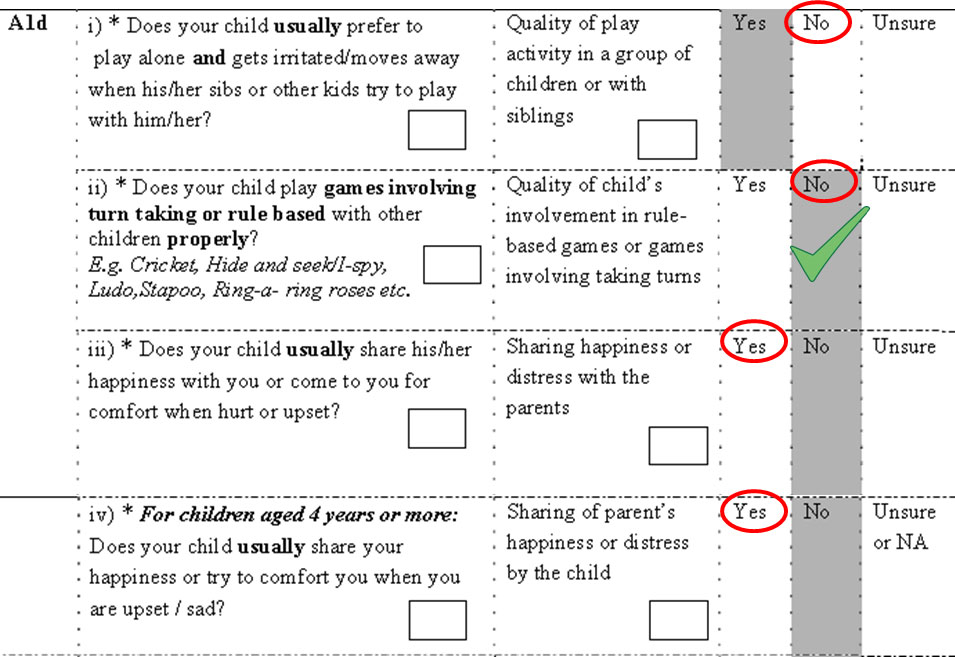
- Some criteria have multiple questions. While scoring, consider the criteria fulfilled even if response to any one of the questions is abnormal. For example, the criterion A1a is considered fulfilled if any one of i, ii, iii, or iv is abnormal in the child.
Observations to Make During Assessment
Clinical Features: What to Look for?
- What is important to remember during an evaluation is that these manifestations vary depending on the developmental level, chronological age and degree of impairment.
Social interaction: What to observe
- The quality of eye contact: absent/ present but ill sustained/ gaze avoidance
- The quality of interaction with the examiner: indifferent/ interactive/ curious/ excessively scared
- The quality of interaction with the parents: indifferent/ interactive/
- curious/ excessively scared/ clingy
- Presence of social smile: present and consistent/ inconsistent/ absent
- Facial expression: blank/ inappropriate expressions
- Response to being touched and cuddled by parent: enjoys/ tolerates/ squirms/ stiffens/ gets upset
- Response to being touched by the examiner: allows examination/ gets upset but allows examination/ starts screaming and does not allow examination
Verbal Communication: What to Observe?
- The quality of language (vocabulary, sentence formation, use of appropriate pronouns and gender)
- The ability to initiate and sustain a conversation
- The pitch, intonation and rhythm of speech
- Look for out-of-context speech, jargon, neologisms, echolalia, unusual sounds, etc
Non-verbal Communication: What to Ask?
- Does the child understand gestures when used during communication?
- Are the gestures used mature (pointing with index finger in appropriate direction) or immature (Pointing with hand without using index finger) or vague (aimlessly and not in the appropriate direction)?
Non-verbal Communication: What to Observe?
- Can the child point to objects, when asked to?
- Does the child look in the direction of the object when pointing at it?
- Is the pointing mature or immature?
- Does the child look at an object when you say’ look at that’ and point to it?
- Does the child ever point out objects of interest to you?
Play: What to Observe?
- Observe how the child plays with different objects and toys
- See whether it is manipulative and functionless or appropriate
- Any form of pretend play
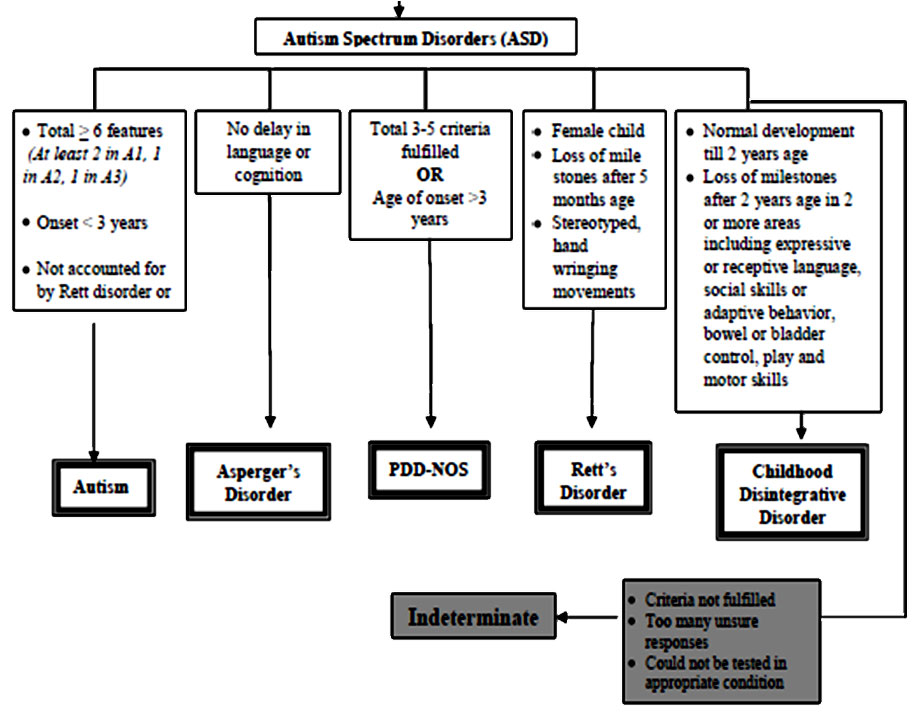
Compare Both The Children
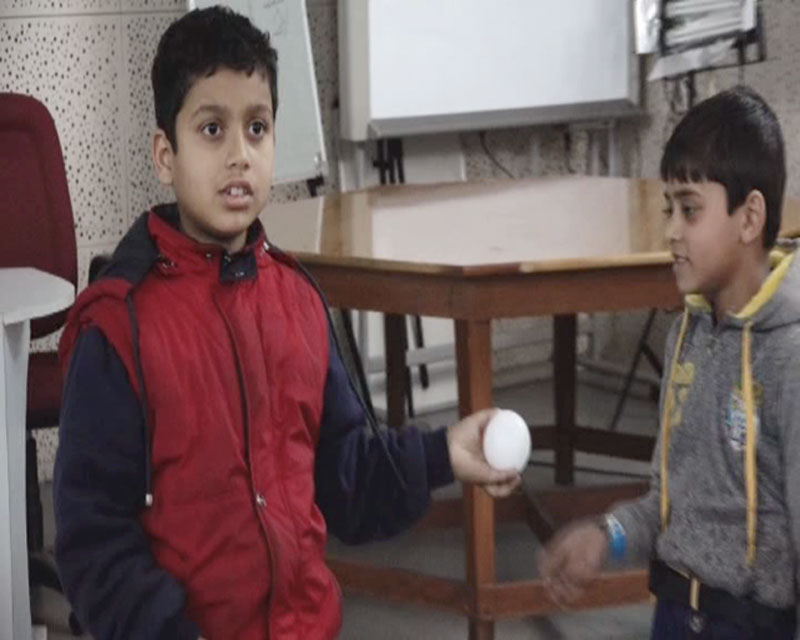
Case Vignette 1
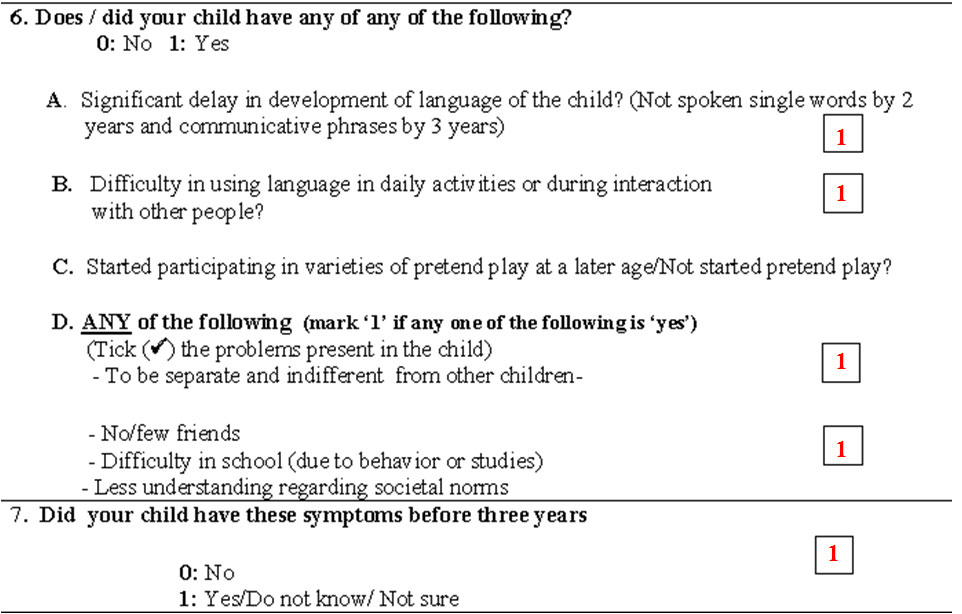
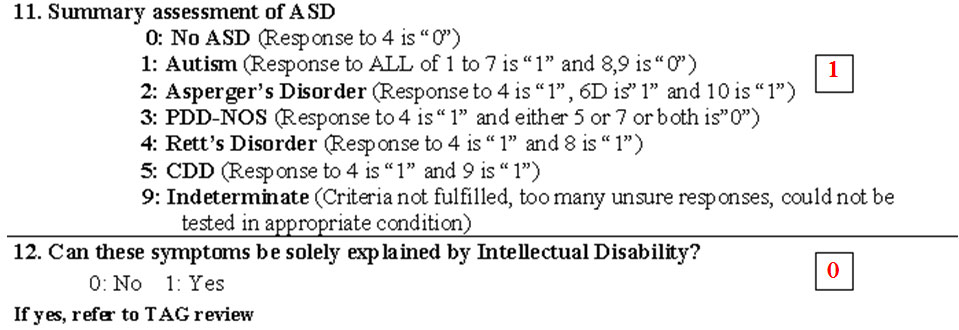
- A three year old boy was brought by her parents with the complaints of delayed speech and abnormal behavior. On further questioning the possibility of an ‘Autistic Spectrum Disorder (ASD)’ was considered.
- The Consensus Clinical Criteria (CCC) for ASD was applied. The parental responses and/or physicians’ observations have been recorded in the form below.
- Give your diagnosis?

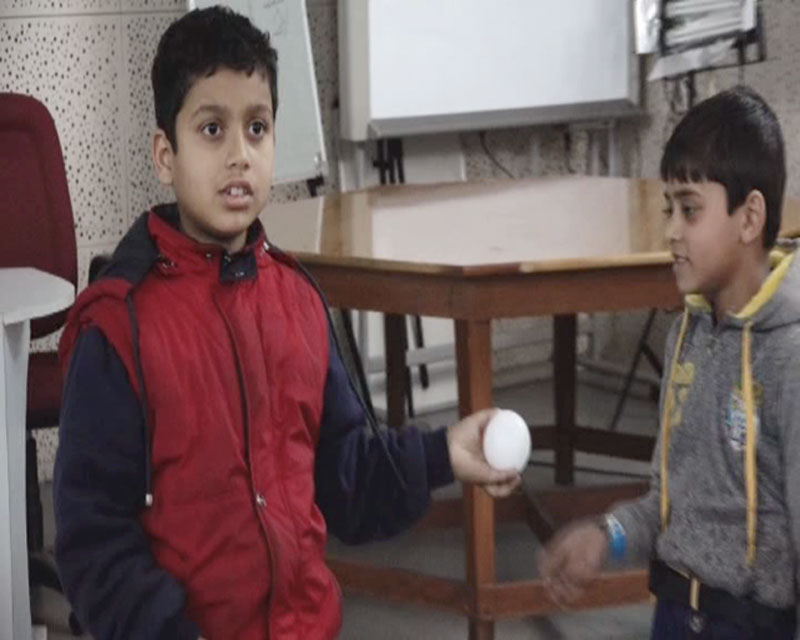
Section A1a
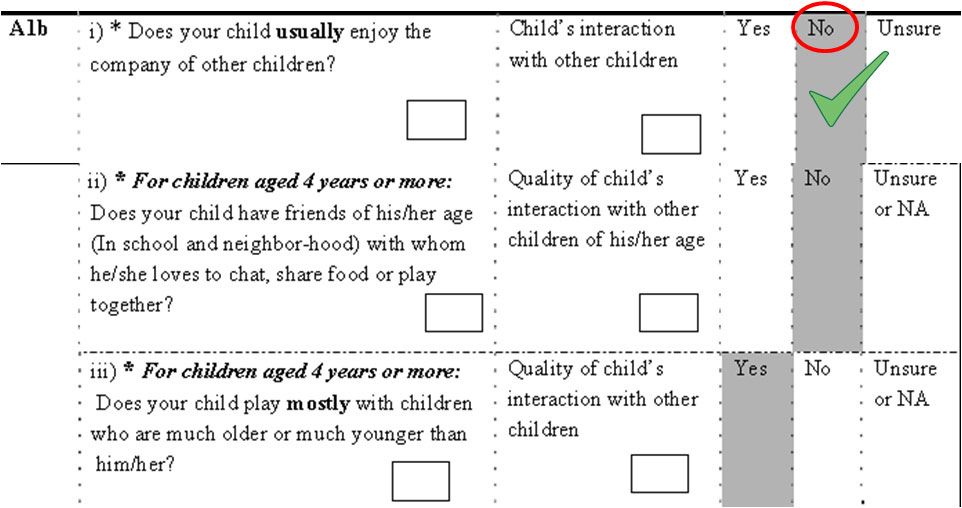
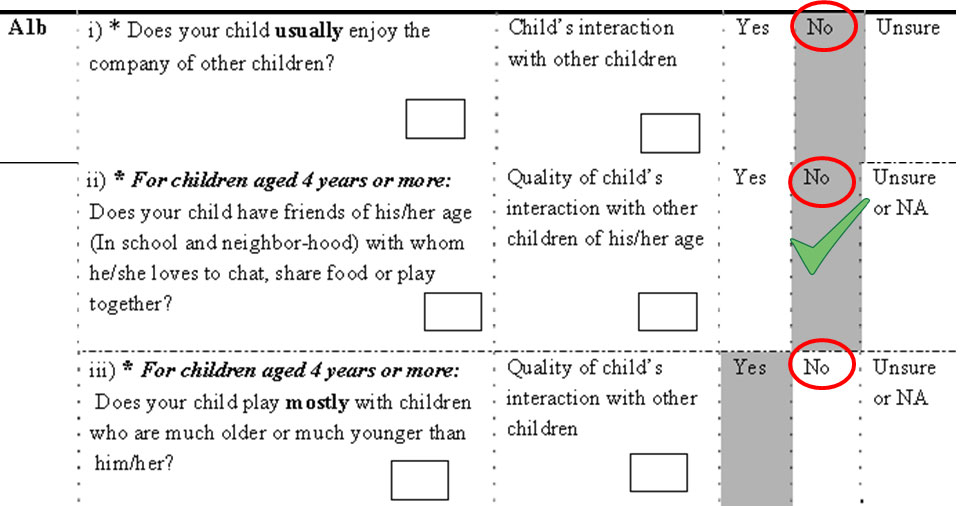
Section A1b
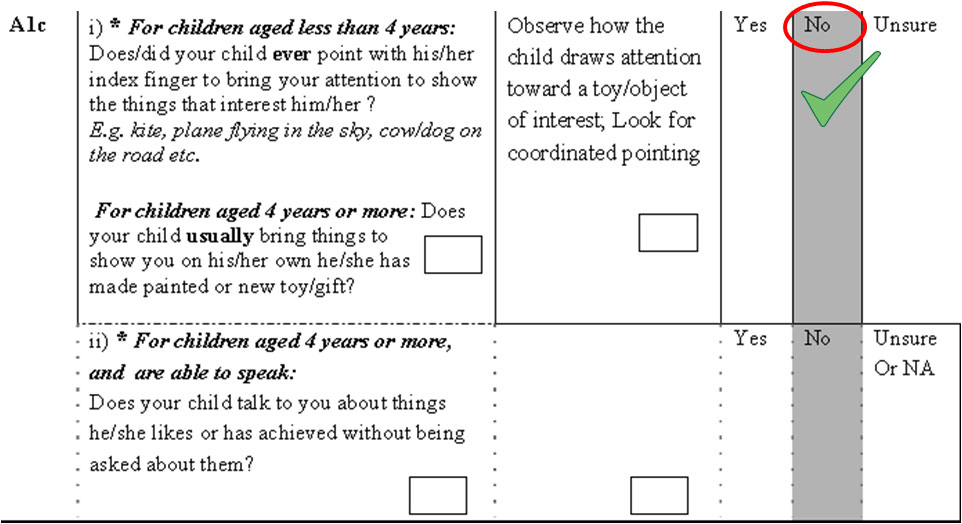
Section A1c
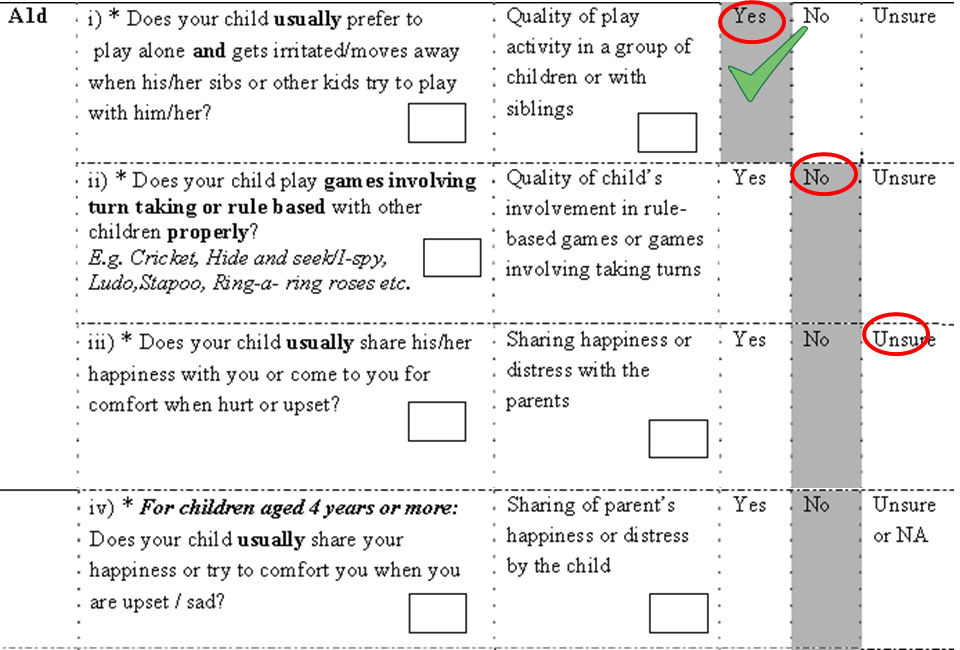
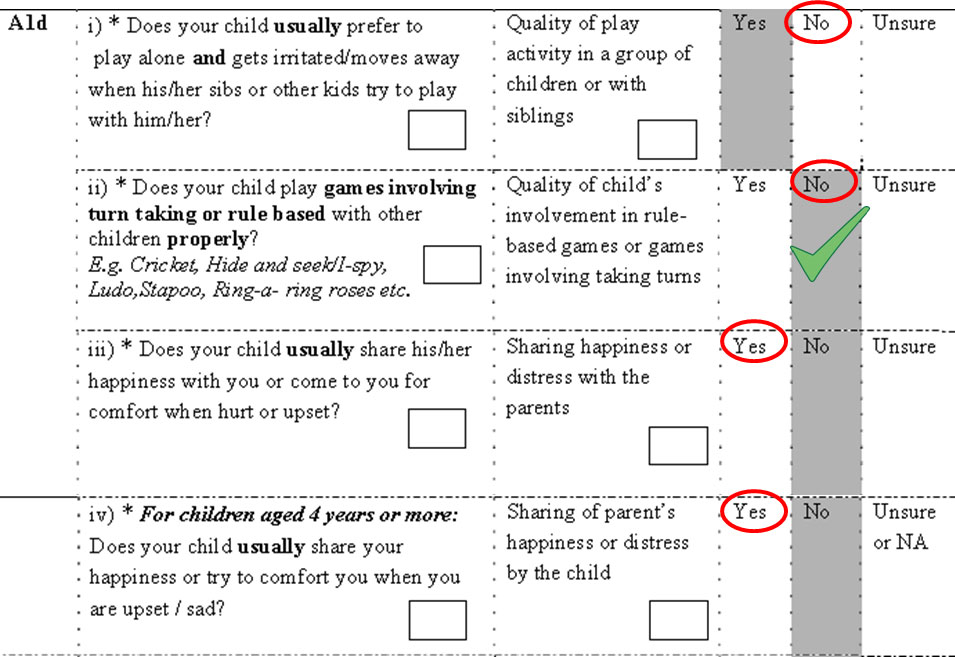
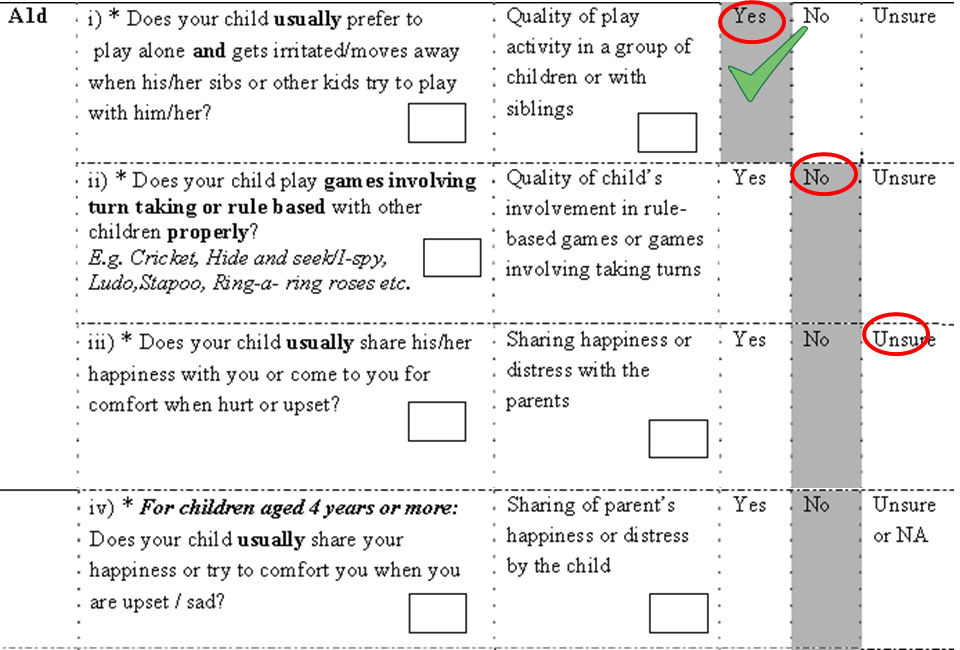
Section A1d
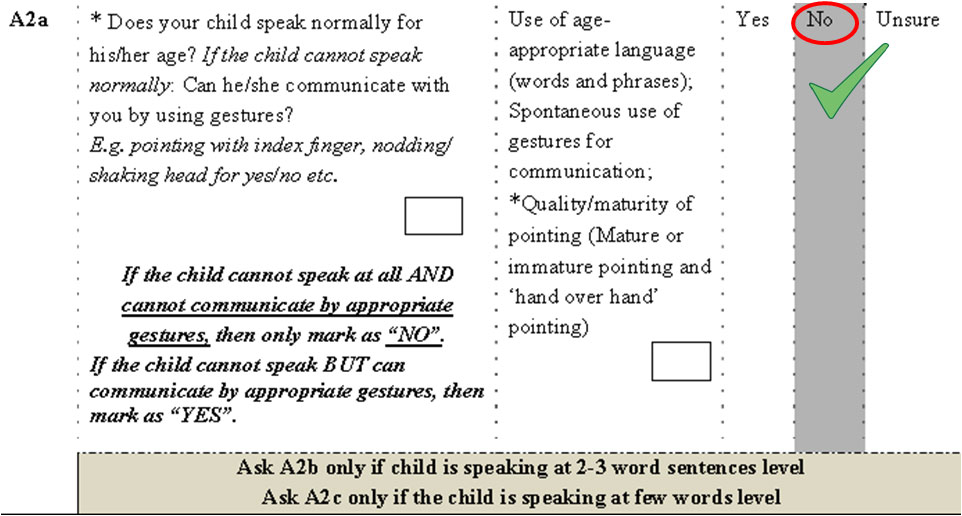
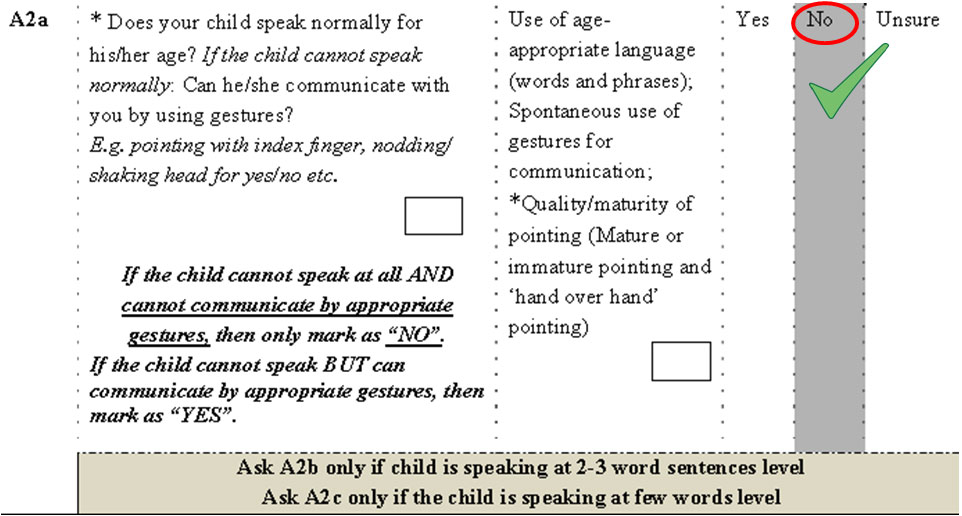
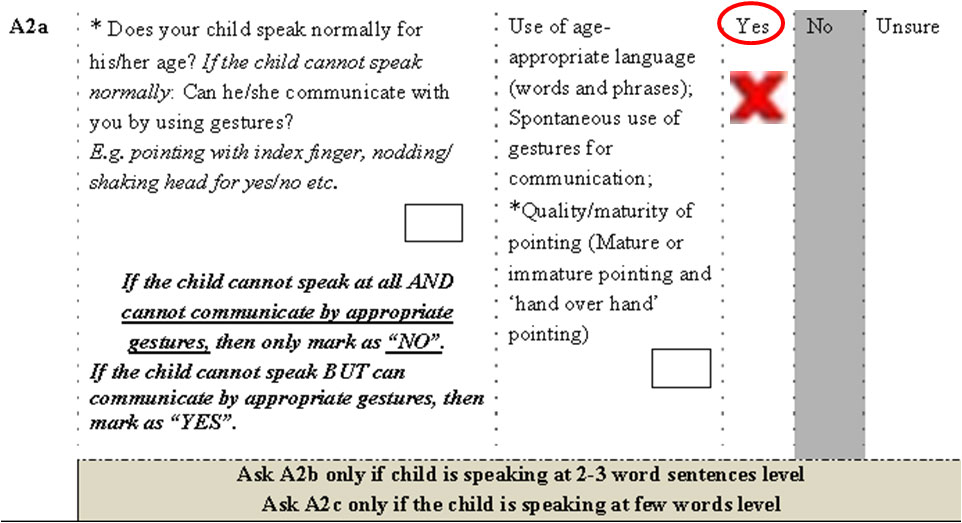
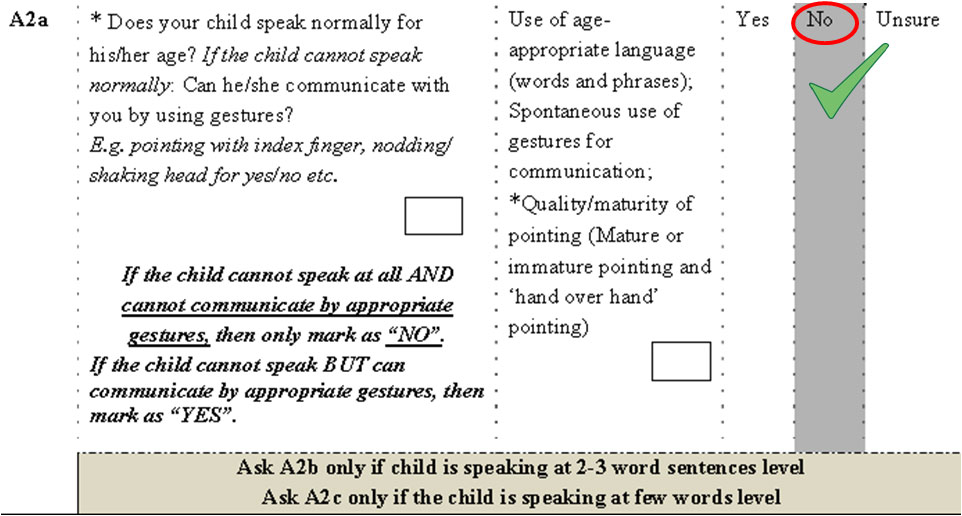
Section A2a
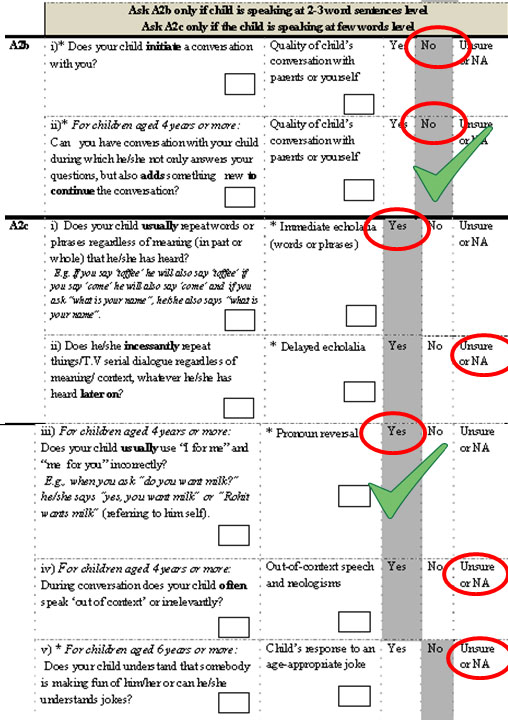
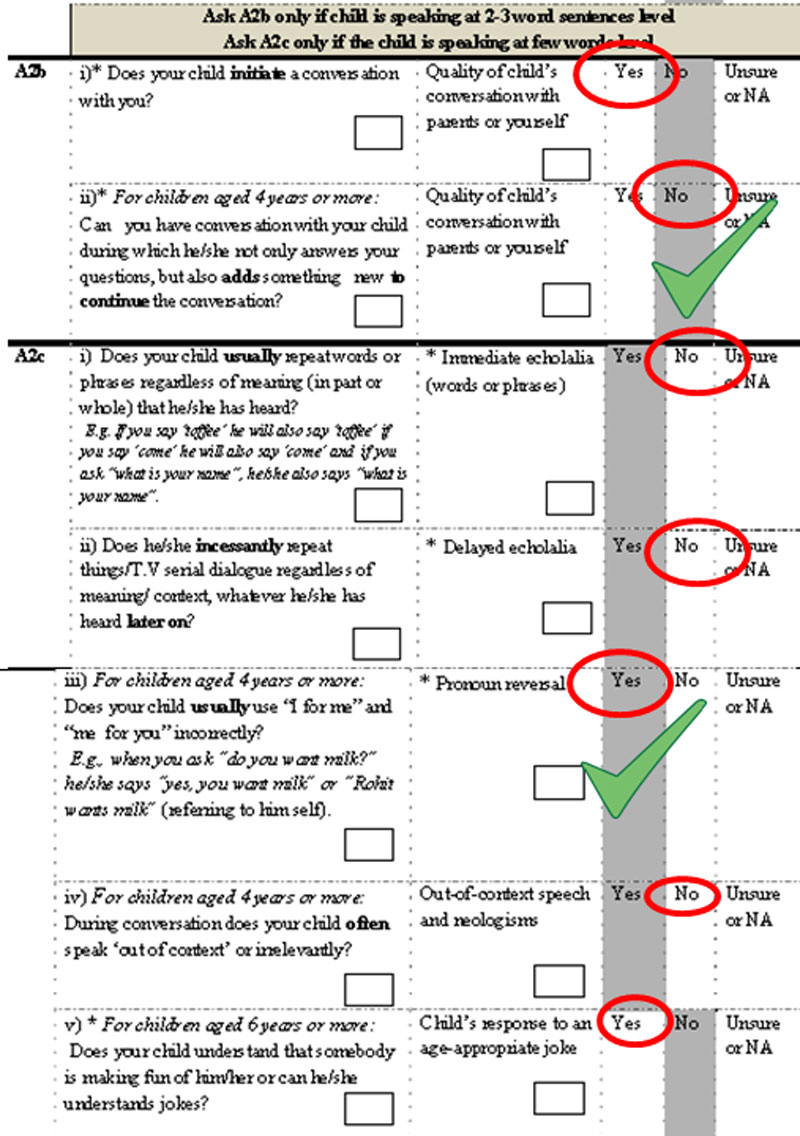
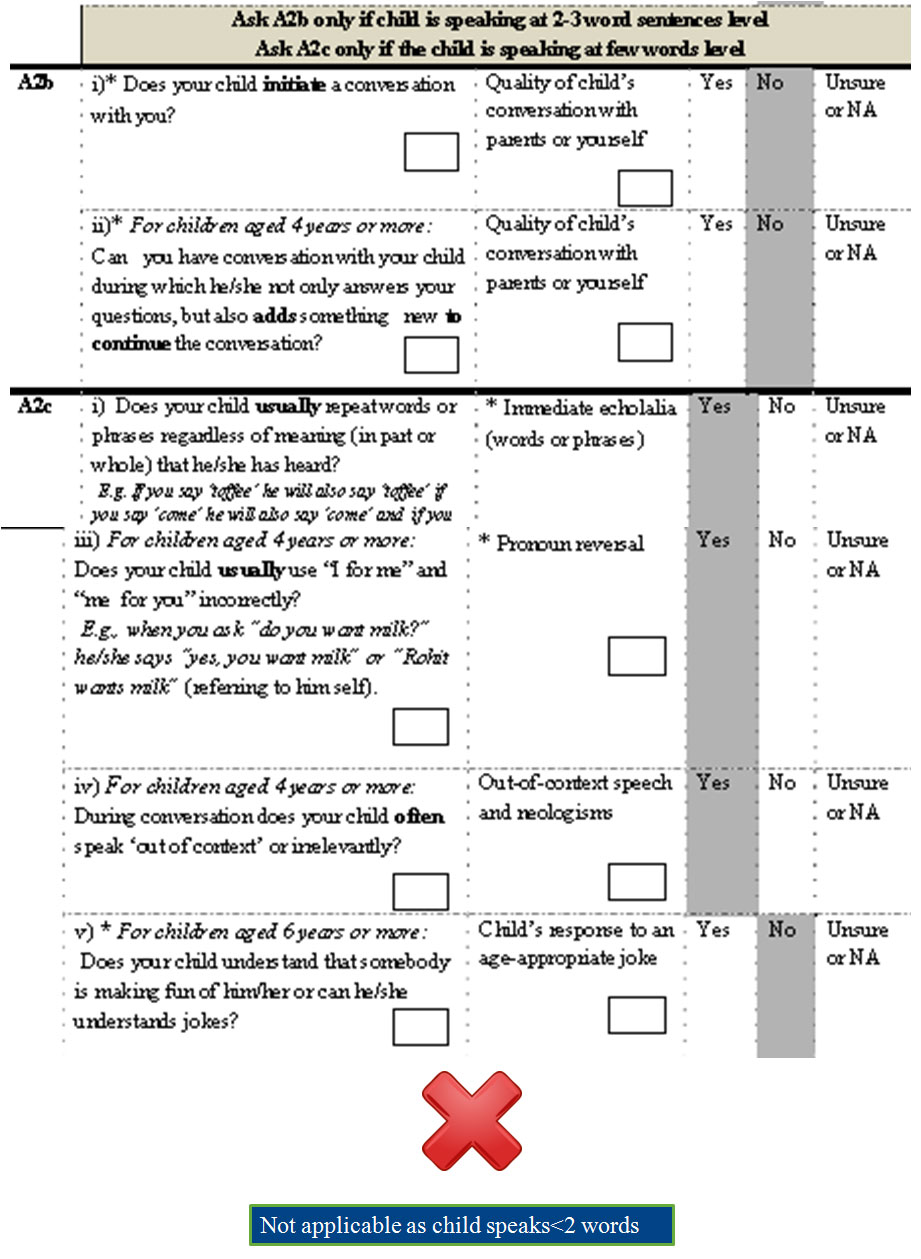
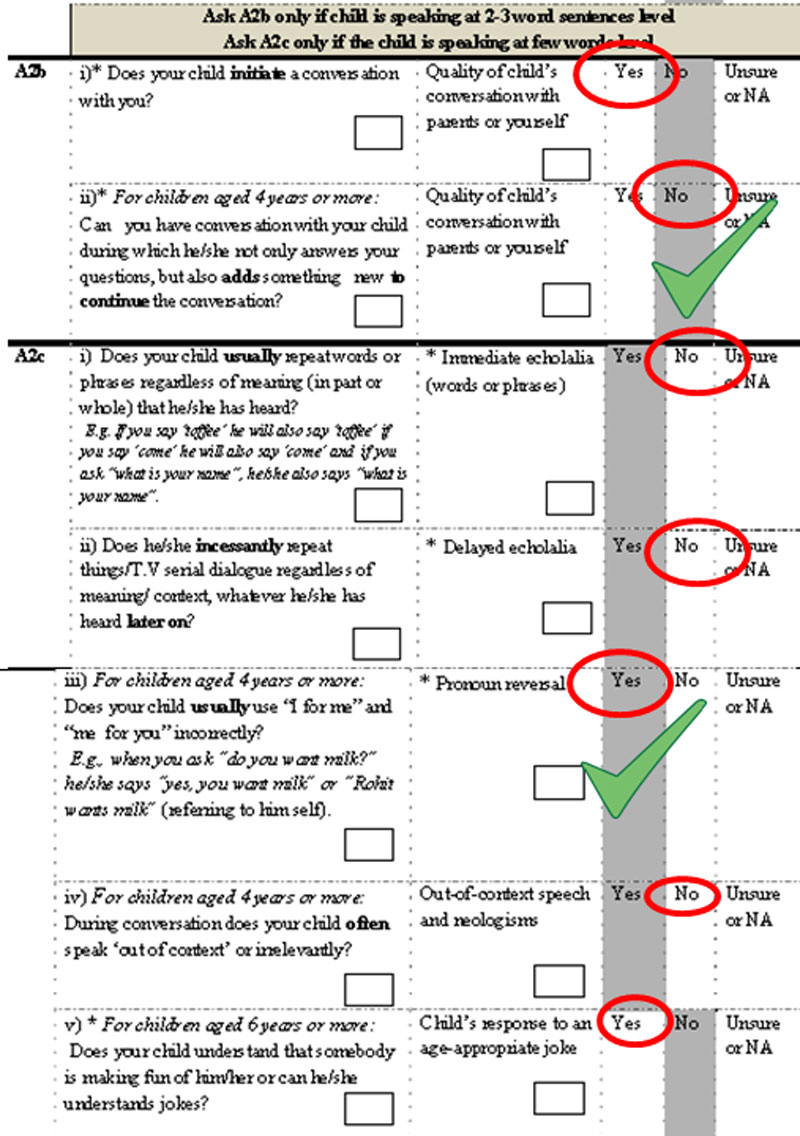
Section A2b & A2c
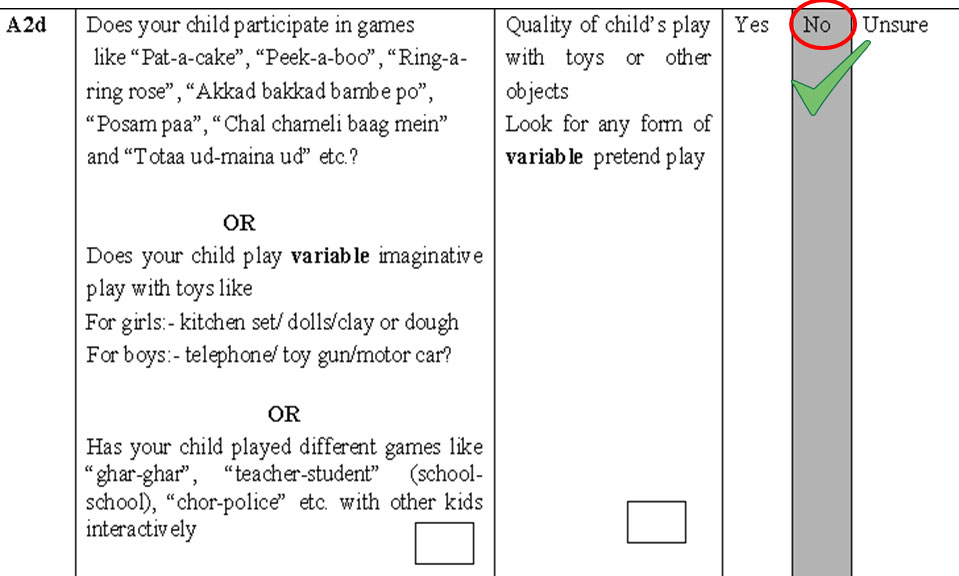
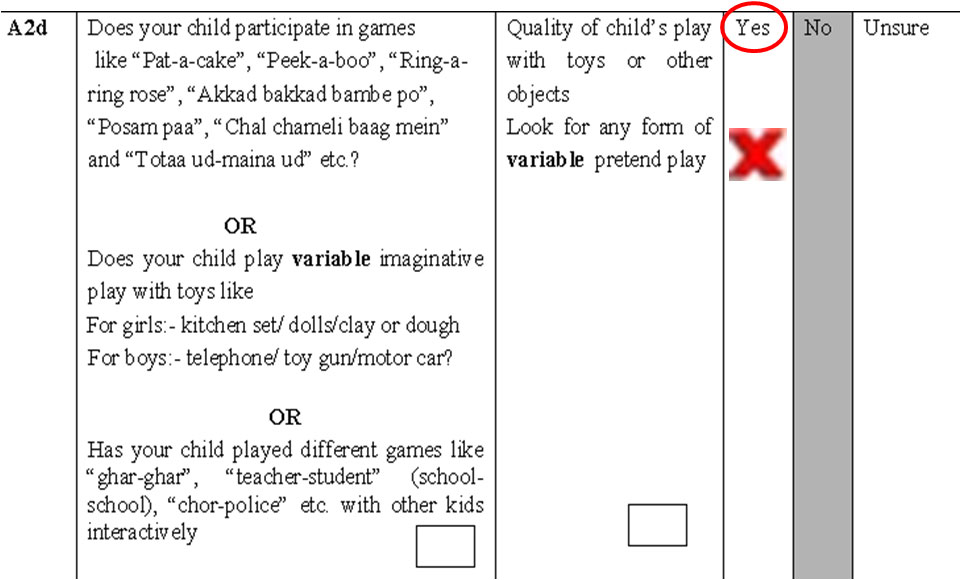
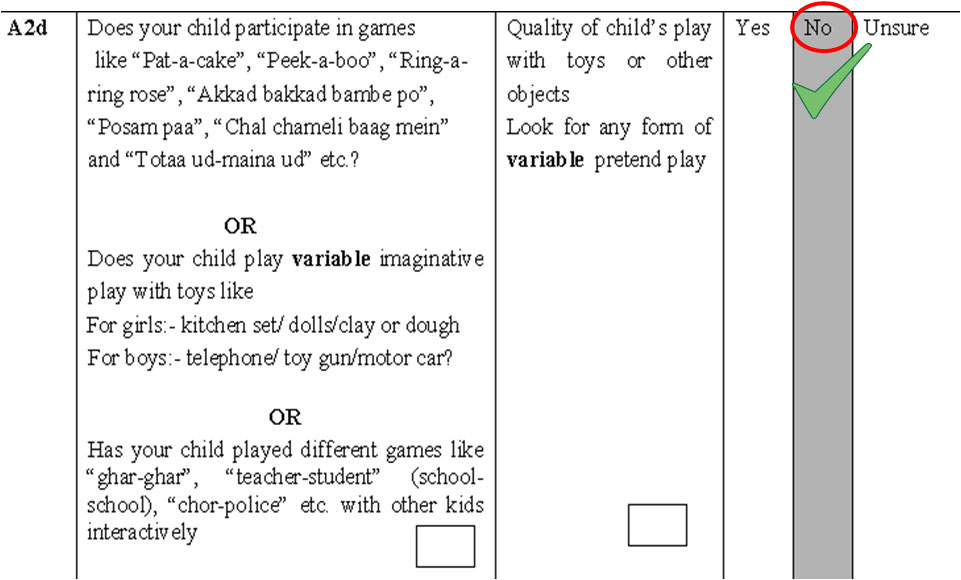
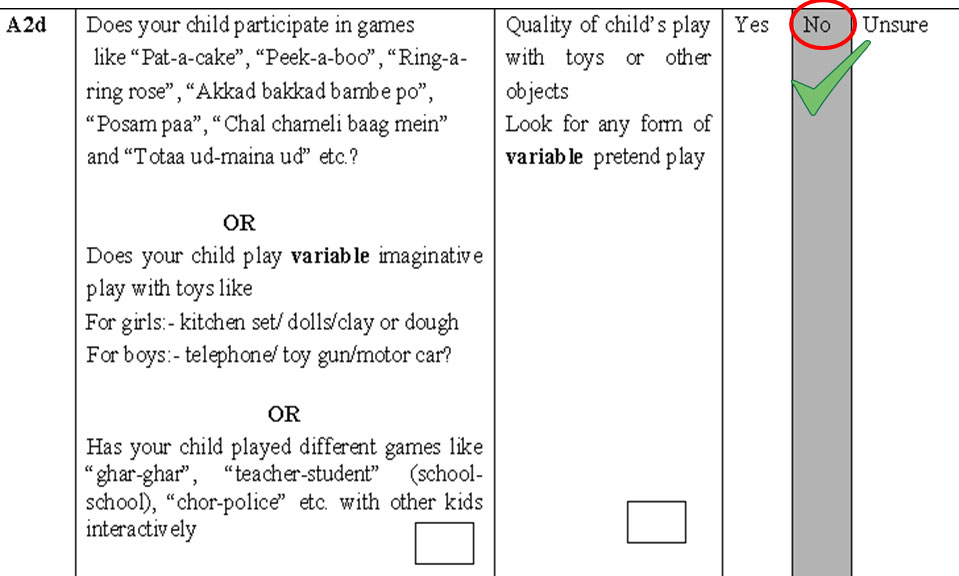
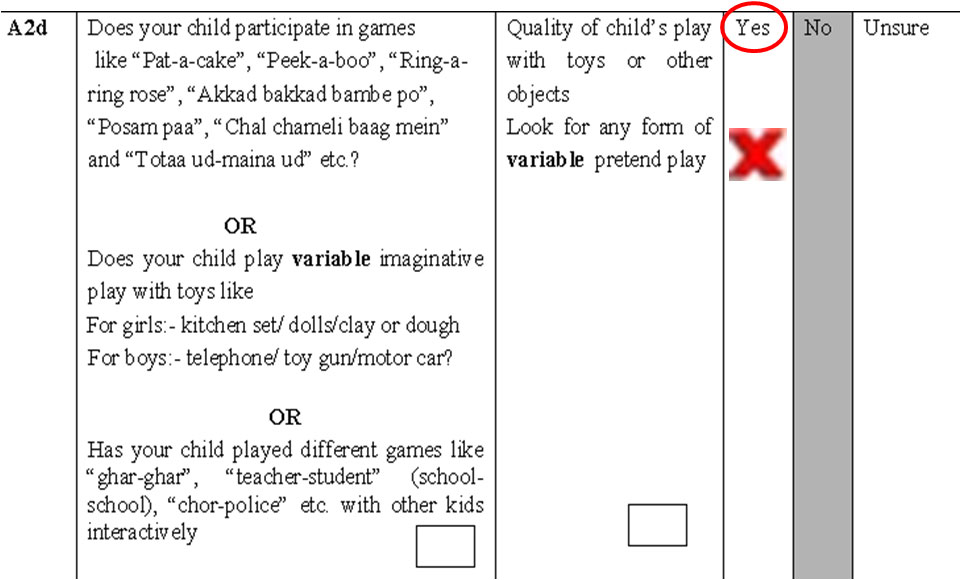
Section A2d
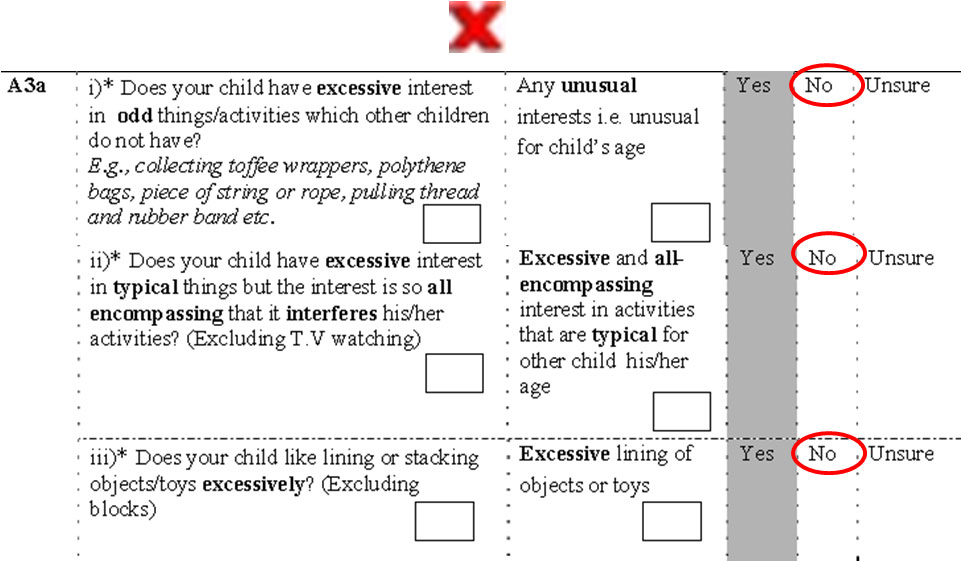
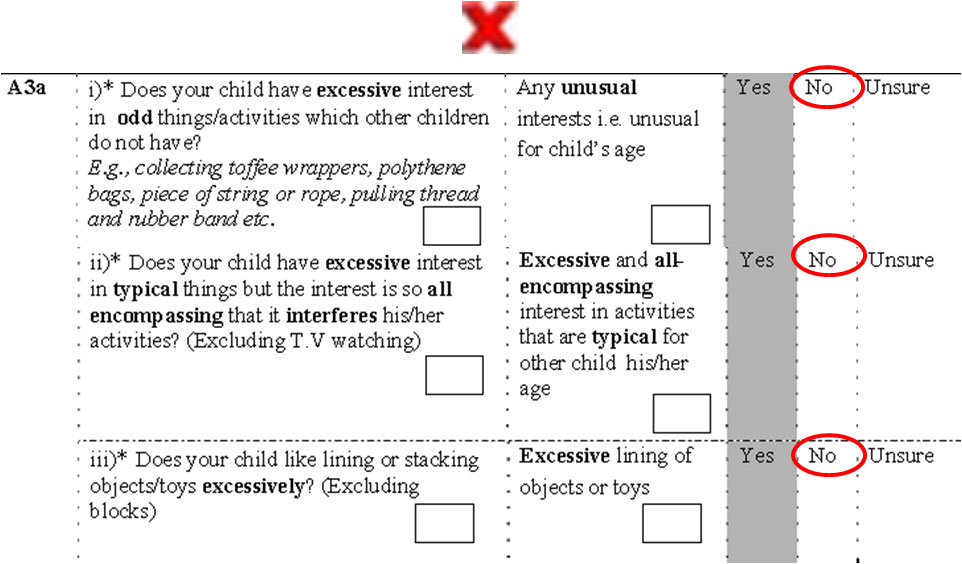
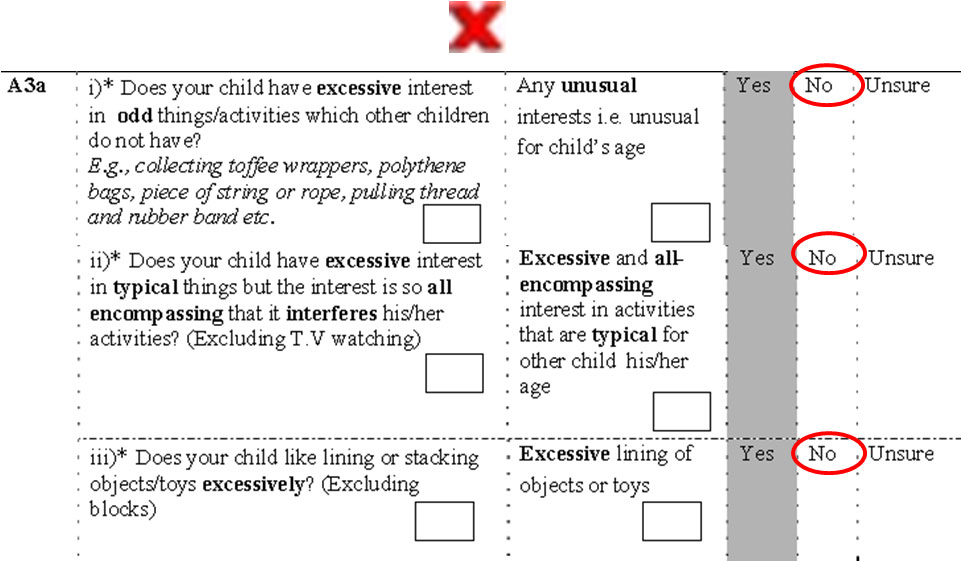
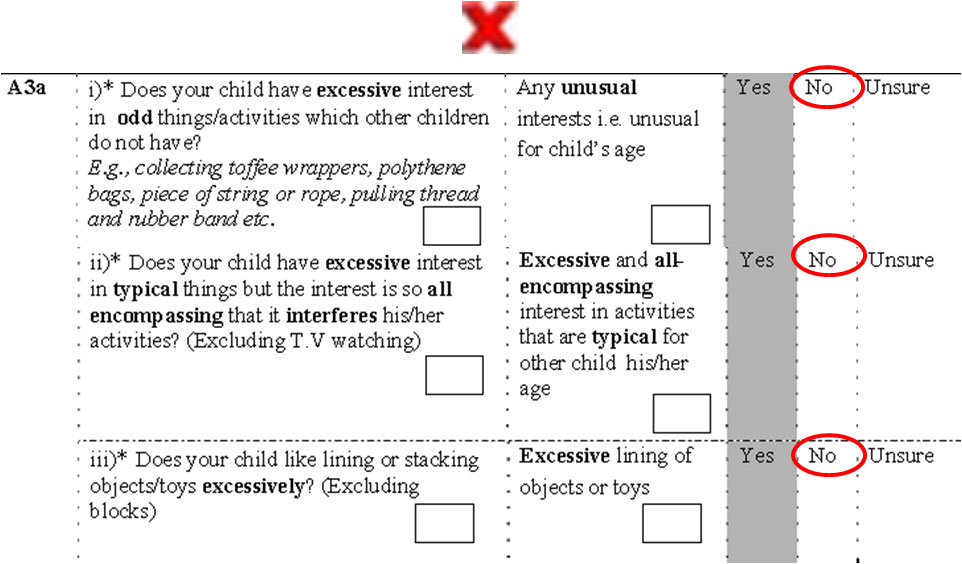
Section A 3a
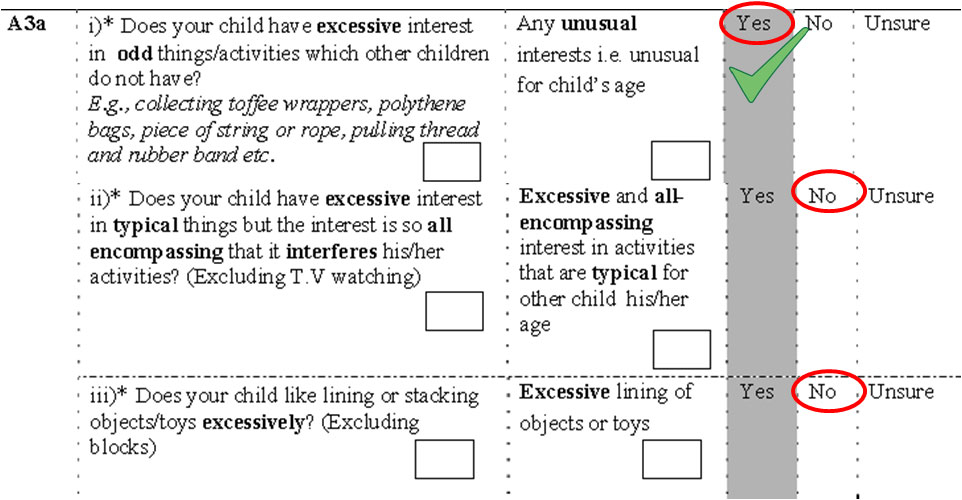
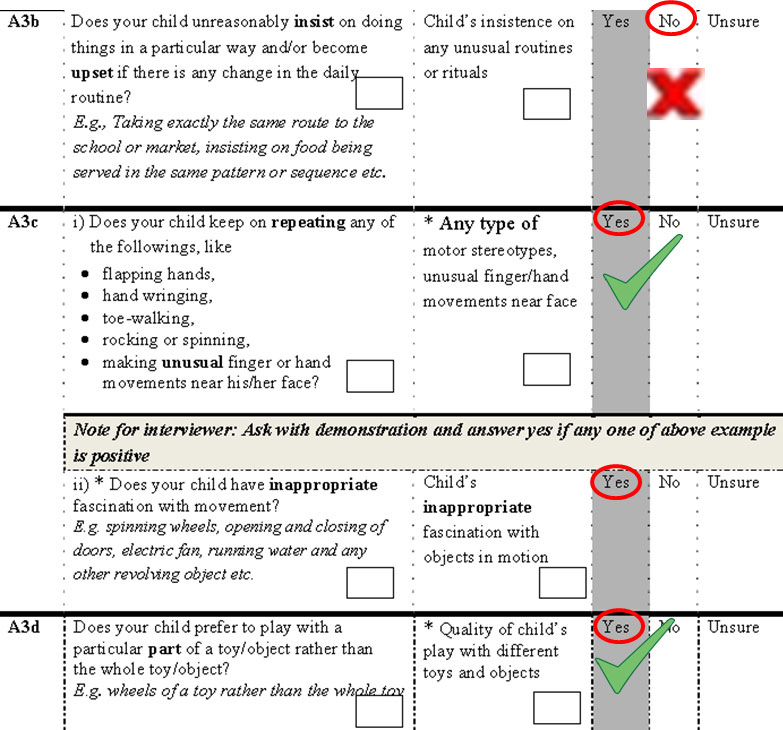
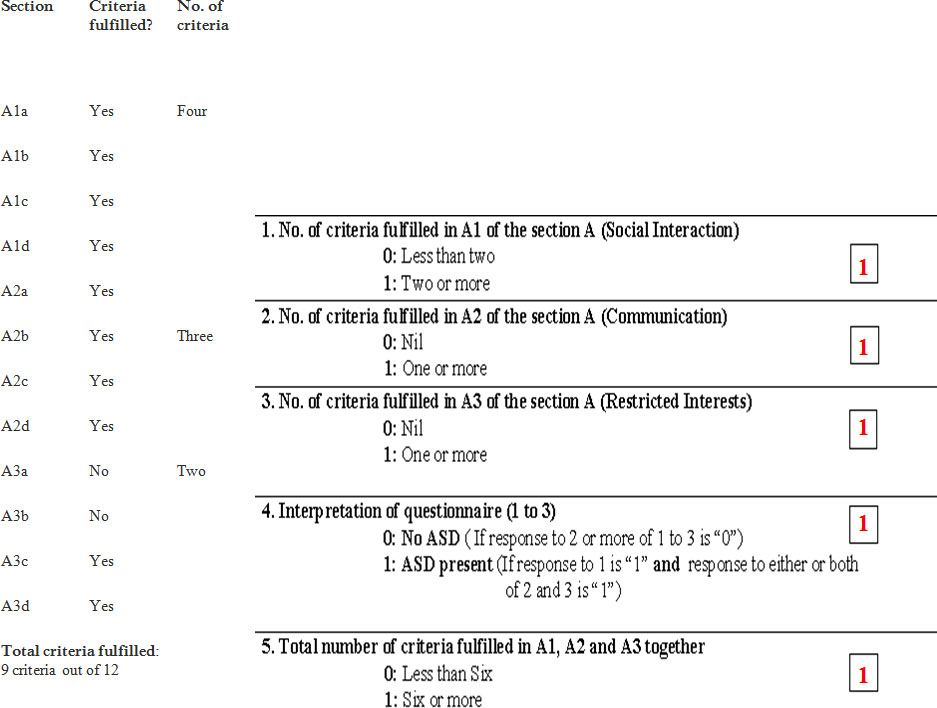
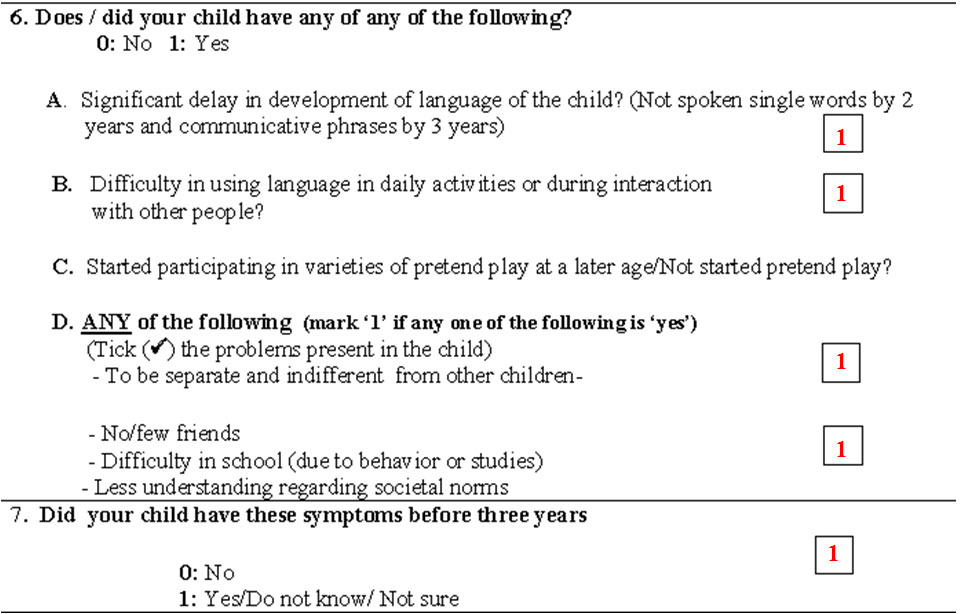
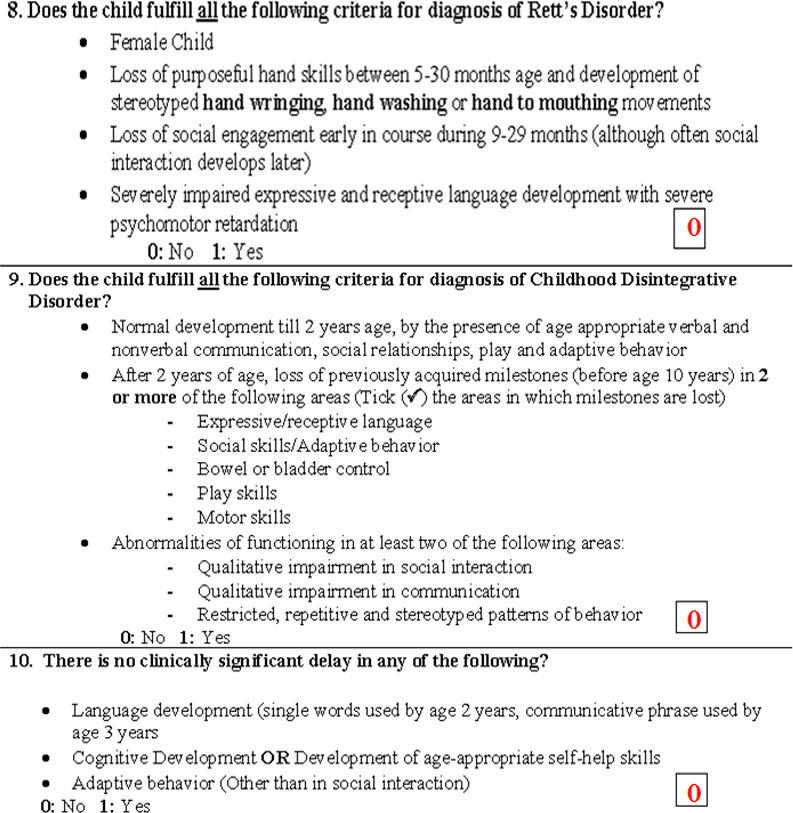
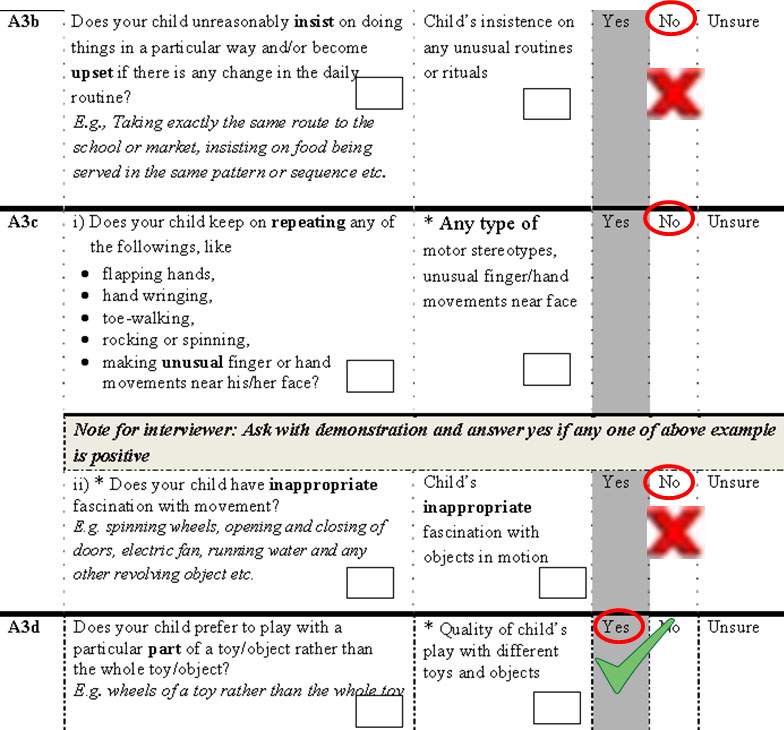
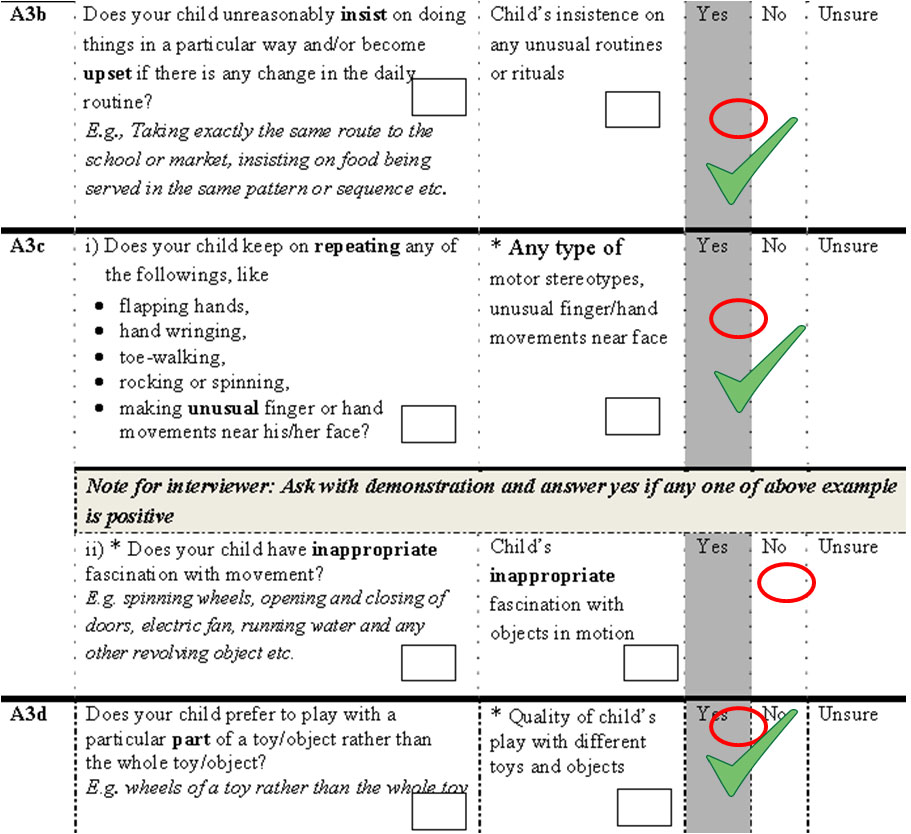
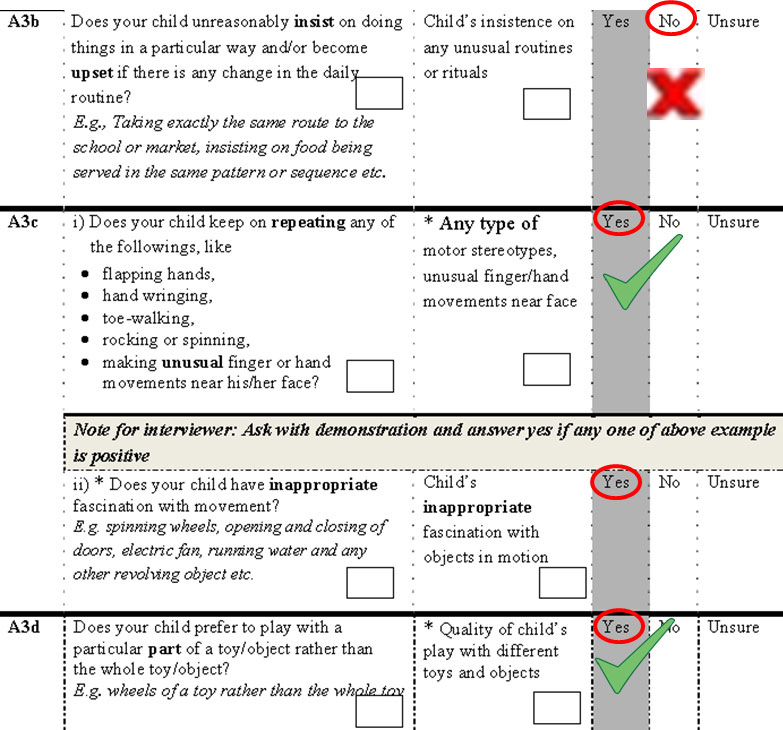
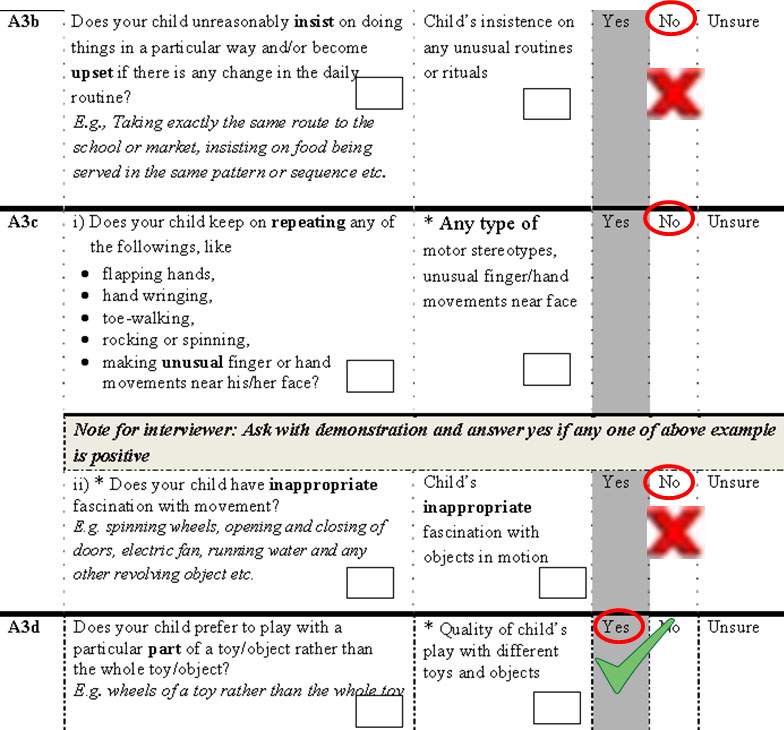
Section A3a, A3b & A3c
Section B
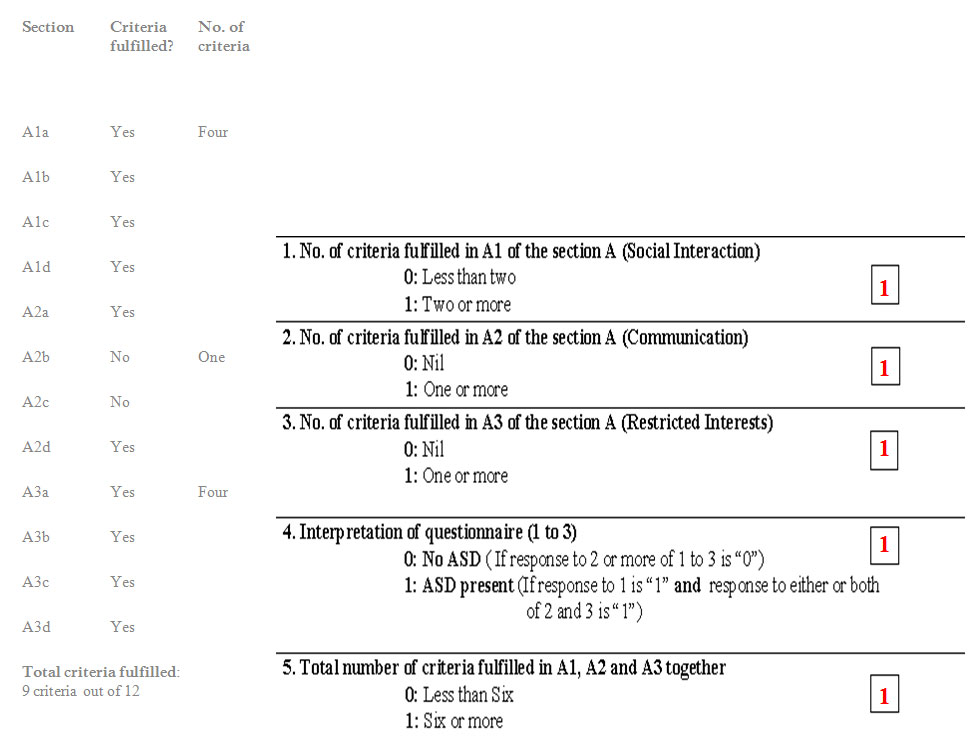
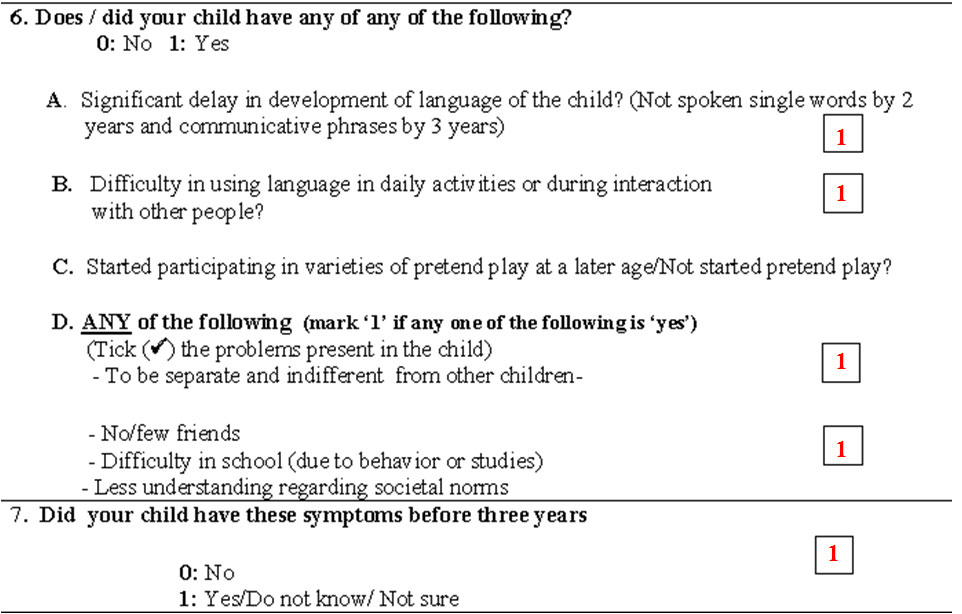
Hence the child is diagnosed to have autism
Case Vignette 2
- A seven years old boy
- Delayed speech development
- Inability to interact properly with children of his own age
- His mother describes him as aloof and is upset because he never enjoys being hugged, and even gets upset when his mother cuddles him on occasion.
- He has never brought anything over to show her or shared anything of interest with her.
- Even when he is in pain or gets hurt he rarely comes to her for comfort, but sits quietly in a corner by himself.
Communication
- He did not begin to speak until the age of three
- Even now uses only about 200 words (mainly names of objects and persons).
- He has not started using pronouns
- Most of his speech consists of repetitive phrases or parts of jingles heard on television, or simple requests or demands
- He is unable to converse properly with others and likes talking to himself in a nonsensical language while rocking back and forth.
- He usually has the same kind of a blank expression on his face, irrespective of the situation.
- He has a tendency of looking away when spoken to
- He does not respond when called
- If he wants to obtain an object that is out of reach he will drag a chair and try to get it by himself or drag an adult to where it is placed and try to maneuver his hand to reach for it He hardly points at objects
- He cannot understand jokes and does not respond when others start laughing at something funny
- His mother complains that he cannot understand simple questions and will give totally irrelevant answers (i.e. what will you eat? - shoe)
Unusual Behaviors and Interests
- He is fascinated with water and often will spend long periods of time intently watching water dripping into a sink
- He shows no interest in playing with toys in a usual way.
- He likes spinning the wheels of a particular red car.
- He would rather arrange objects like kitchen utensils in a straight line. He can do this for hours on end.
- His play never exhibits any sort of variety or use of imagination.
- He shows little interest in usual children’s programs or cartoons on television; but likes watching programs with fast music.
- He becomes very upset if things are changed in the house and was inconsolable when his parents bought a new car
Social Interaction
- He does not interact much or communicate with his nursery teacher
- She is concerned as she has observed that he prefers to stay by himself, rather than play with other children
- He has not made any friends and becomes irritable if other children try to approach him

Observations
- He has minimal communication skills
- Did not use any gestures at all throughout
- He did not follow the examiner’s finger when he pointed at a toy in the corner of the room
- He muttered some unintelligible words in between to himself and did not react to any of the examiners questions (i.e. Where is your mother? Show me the fan, Come here.)
- He repeated a few words of the questions that were asked of him
- He did not exhibit any interest in the few toys that were there in the clinic
- He made a line of the toy cars by placing them in a line against the wall
- He spun the wheels of his red car for around 10 minutes at a stretch
- No form of pretend play was noted
- Toe-walking
- Rocking from side to side
- Frequent unusual hand movements near his face (his mother had not noticed him making this at home)
- He kept on getting up and moving around the room
- He went to the door quite a few times
- At departure he did not acknowledge or wave back to the examiner.
Study the given case and apply the CCC to make your diagnosis?
Section A1a
Section A1b
Section A1c
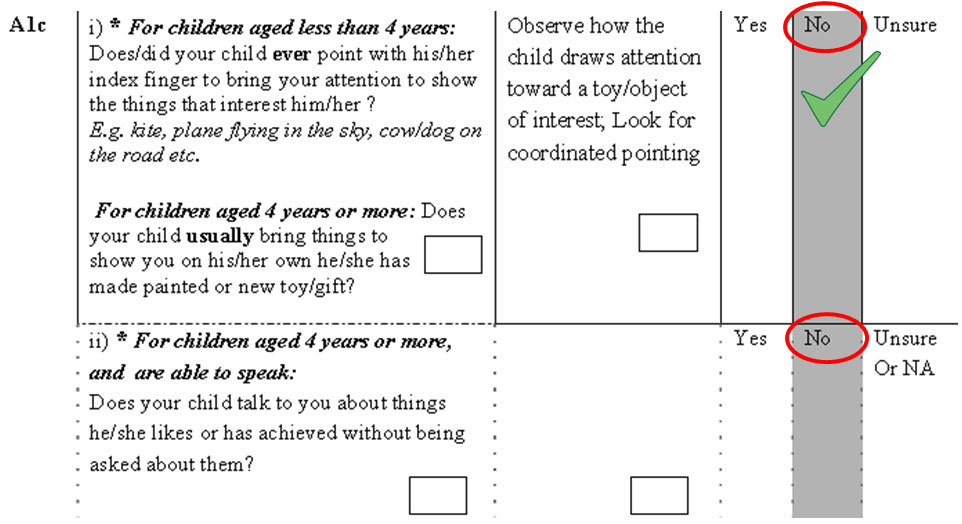
Section A1d
Section A2a
Section A2b & A2c
Section A2d
Section A 3a
Section A3a, A3b & A3c
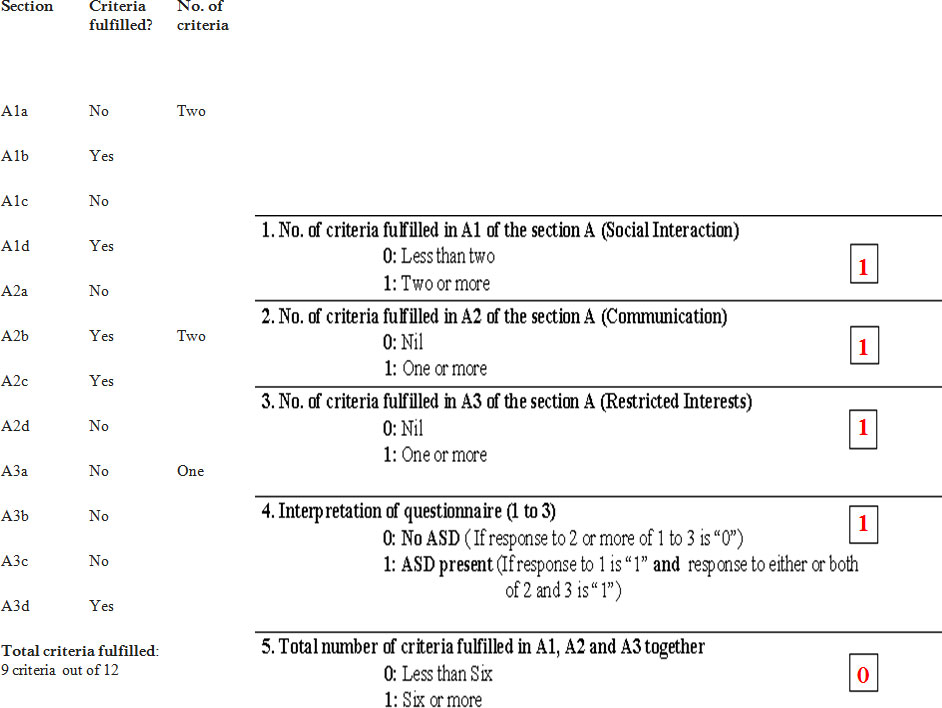
Section B
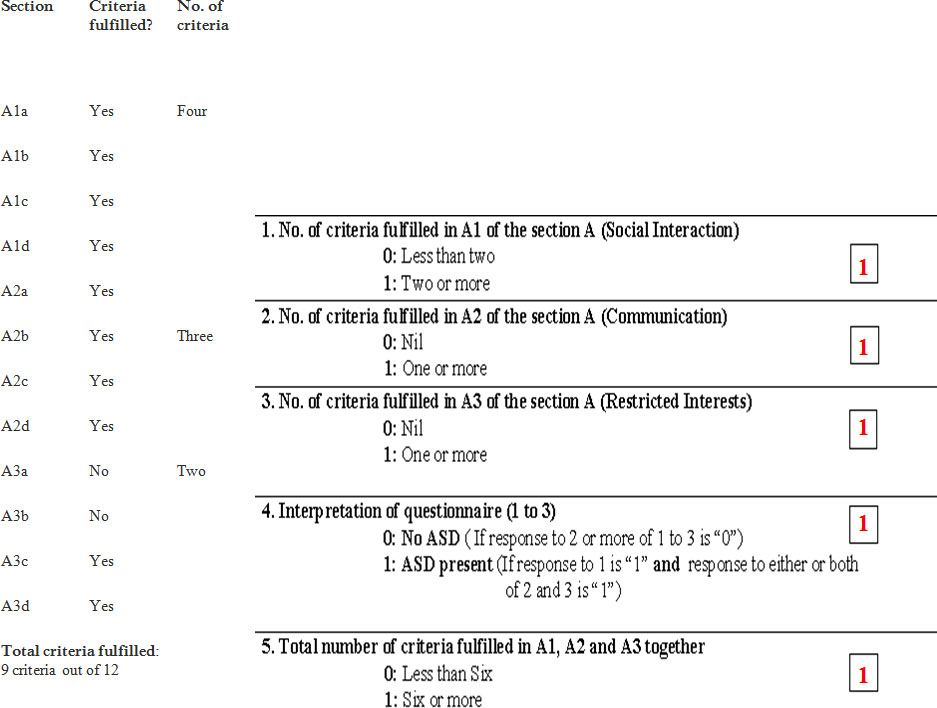
Hence the child is diagnosed to have autism
Case Vignette 3
- A seven year old boy studies in class 2.
- His mother has started becoming concerned at his inability to make friends with children his own age, although he seems to get on well with much older children.
- He is extremely shy with adults as well, but can be made to interact with a lot of persistence.
Complaints
- He never played with toys a lot except for all sorts of mechanical and clockwork toys, which he likes taking apart and reassembling.
- He will show his parents his handwork and is happy when they applaud.
- He sometimes pretends that he goes to work like his father, who is an engineer and is extremely proud of this particular talent.
- He likes collecting screws and nuts in a polythene bag, which he carries in his pocket all the time. He gets extremely upset if he is asked to leave them at home.
- He usually doesn’t like playing games, but can be persuaded to play with some insistence
- His mother is also concerned that he does not speak as much as children of his own age.
- He can carry out a conversation when he wants to, but he is usually not so inclined.
- There was a slight delay in attainment of language in early childhood, which led him to being screened for a hearing deficit. However he was found to have normal hearing.
- He displays some unusual habits on occasion.
- He likes rocking from side to side, especially if he has nothing to do.
- When he gets excited he occasionally flaps his hands.
- His mother has seen him walk on his toes at times, which she thinks is a game they play at school.
- His performance is average at school and there are no complaints regarding his behavior.
- The child does not seem to be sad or depressed and there are no family problems at home.
Observations in Clinic
- He seemed to be shy.
- He gave a slight smile in response to the examiners greeting but said ‘hello’ only after prompting by his mother.
- His eye contact was sustained and changes in his expression were noted.
- It was very difficult to draw him out.
- He didn’t speak much, although he responded appropriately (but very briefly) to whatever was asked of him.
- He showed the examiner his little back of screws, which he was carrying in his pocket.
Observation
- There were no overt speech abnormalities, although there was definitely decreased speech on the whole (without the presence of resentment or irritation).
- He responded to a joke cracked by the examiner after a slight delay.
- He only displayed interest and played appropriately with the battery-driven car with a degree of pretend play as well in the form of noises and planning of destination.
- No stereotypic movements were observed.
- His anthropometry (including head circumference of 51.5 cm), general physical examination and systemic evaluation are normal.
Apply the consensus clinical criteria to the aforementioned case and make your diagnosis
Section A1a
Section A1b
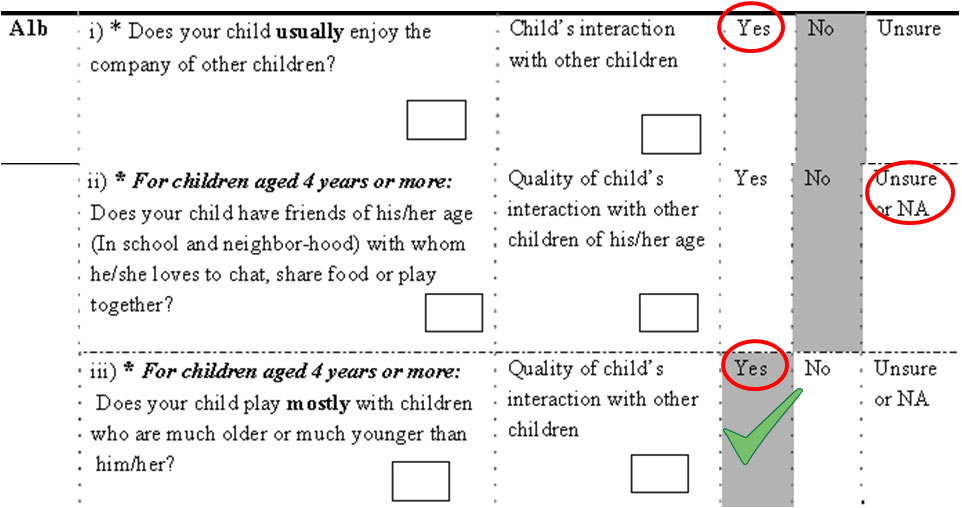
Section A1c
Section A1d
Section A2a
Section A2b & A2c
Section A2d
Section A 3a
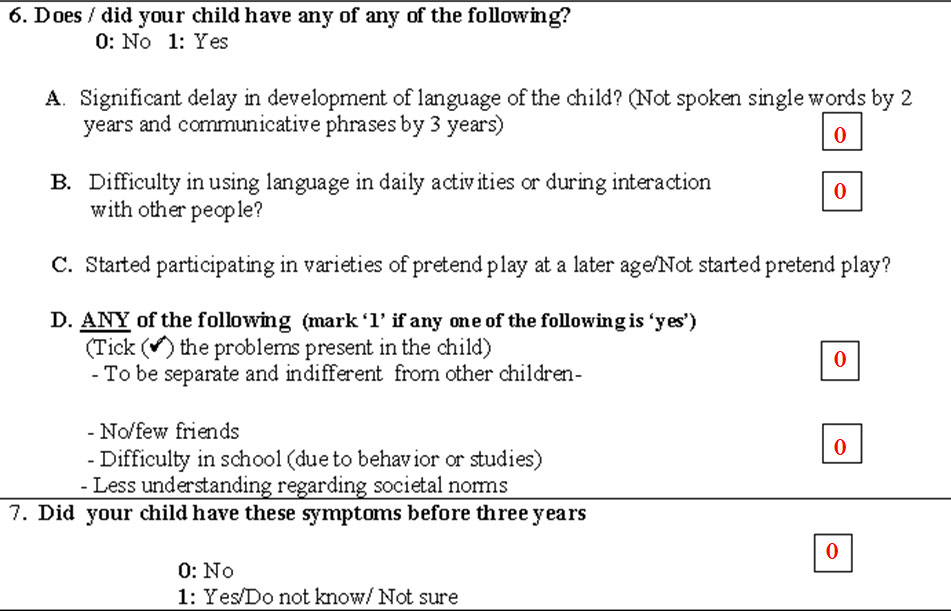
Section A3a, A3b & A3c
Section B
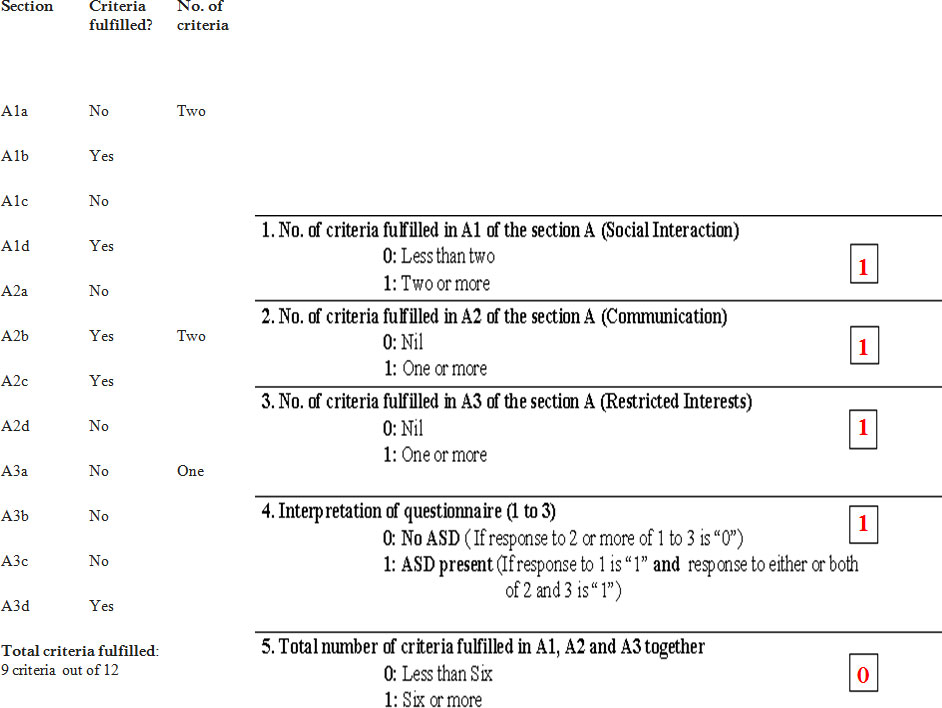
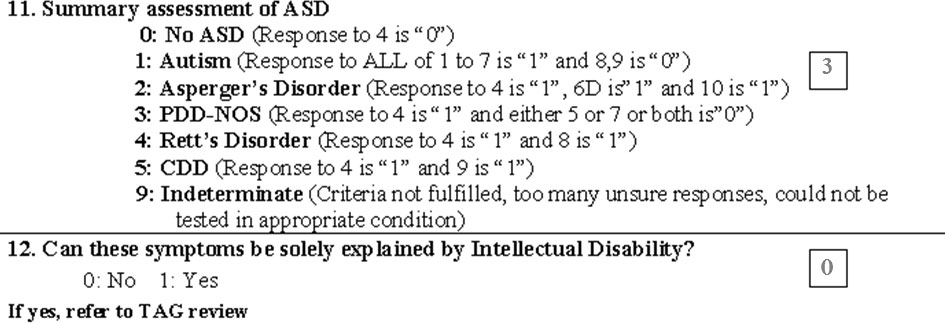
Hence the child is diagnosed to have PDD-NOS
Conclusion
- Autism spectrum disorder is a common neuro-developmental disorder
- Early diagnosis and early initiation of behavioral therapy could be useful
- INDT-ASD is good Indian tool for diagnosis of autism
- Need for further research and development of Indian tool based on DSM-5
Thank You